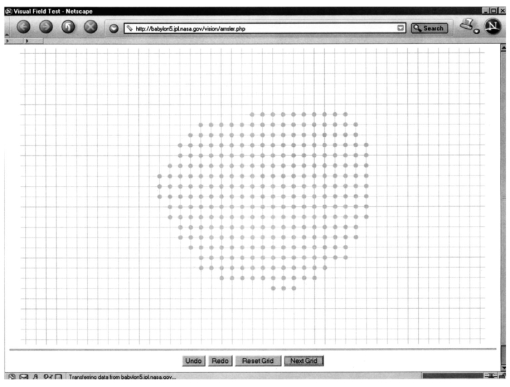
1.IntroductionThe assessment of resolution, generally described as visual acuity, has traditionally been the cornerstone of an examination of the visual system. Snellen1 introduced letter optotypes in the 1860s and although there are theoretical reasons for choosing other measures of angular resolution, the user friendliness of this traditional method has left this as the standard. However, this assessment is, almost by definition, only a very tiny piece of the puzzle. Snellen acuity captures only one parameter of vision in approximately four square degrees of central vision. Not only is Snellen acuity capturing less than 0.1 of the visual field but in addition fails to take into account several other parameters of vision, such as contrast sensitivity and color vision. Hence, despite its clinical popularity, most investigations of visual function employ variations of Snellen acuity and do so in conjunction with several other parameters of visual function. Some forms of visual field testing preceded Bjerruns work; however, he brought quantification to the assessment of the visual field using black velvet tangent screens in conjunction with targets of different sizes and illumination. Traquair and Goldman introduced greater sophistication in these assessments of visual fields over the next 60 years. However, Traquair also provided an ideal analogy for understanding these concepts. He described “an island of vision in a sea of blindness.”2 This of course introduces the concept of three dimensions. The single high point in the middle of the island represents vision at a fixation where retinal sensitivity is at its highest. At this point even weak stimuli can be detected. As one proceeds eccentrically from the central mountaintop, the elevation diminishes, reflecting decreased retinal sensitivity. At the water line, or perimeter of the island, only the strongest stimuli can barely be seen and then the sensitivity drops off to undetectable. This analogy also offers us the best understanding of the differences between kinetic and static perimetry. In the former, a strong stimulus begins peripherally and is moved centrally until it hits against the island at a known elevation. Mills3 describes this as airplanes flying toward the center of the island and crashing about a perimeter peripherally. Note that this is the principle involved with Bjerruns tangent screen testing or in Goldman perimetry. In contradistinction, static perimetry consists of exploring the elevation at any known location (with longitude and latitude fixed). Mills again refers to the island of vision as an analogy and says that this would be like dropping parachutes without the use of a timer and then noting the height at which each parachute lands. This of course establishes a contour map of the island. Static perimetry, by giving us this elevation, provides the threshold or establishes the sensitivity of the retina at a number of preselected sites. One great advantage of perimetry is that it would disclose any irregularities that might take us away from an island that would seem like a perfect volcano emanating from the sea. Hence ridges, depressions, pits, and other contour variations might be determined by looking down at the island from the air (e.g., parachuting) and yet would not have been disclosed by simply establishing the perimeter of the island. On the other hand, static perimetry is very tedious for the examiner and examinee alike. A great deal of time must be employed in testing with stimuli that are either way above the threshold or way below and, partly in compensation, a great deal of extrapolation must be made using the relatively few location points tested. In short, static perimetry does not lend itself to high-resolution testing of the visual field. Small scotomas are missed in this type of testing, just as centrally located irregular depressions are missed by kinetic perimetry. Amsler4 5 developed a series of charts in the 1920s designed to assess visual function specifically in the central 10 deg of vision. By displaying this gridlike pattern and asking the patient to record abnormalities, he achieved great economies in expense and time. Although Amsler grid testing can be done with a variety of colors and backgrounds, it is commonly performed with black lines of a 1-deg separation against a white background. This, of course, would be a suprathreshold test (100 contrast) and patients would only note absolute scotomas (areas at which the retinal sensitivity was near 0 and they could not see at all). An area of decreased retinal sensitivity can still be stimulated with 100 contrast. In 1986 Wall and Sadun6 suggested that the Amsler grid test could be modified to measure threshold levels. This testing was done in conjunction with cross-polarizing filters that varied the perceived luminance. That is to say, the filters would be rotated so that the lines in the background became harder to distinguish and titrated just to the point where the grid could be barely discerned. At this point even a small dip in retinal sensitivity would make the patient aware of the area in which the lines disappeared, and this could be noted. This threshold Amsler grid testing technique increases the yield of scotoma detection about the central 10 deg as much as sixfold over standard Amsler grid testing. This technique also proved to be superior to static and kinetic tangent field testing, automated visual field testing, etc.6 Taking this a step further, Fink and Sadun7 8 in 2000 integrated threshold Amsler grid testing into a computer-automated form (Fig. 1). In addition to threshold stimuli, increasing levels of contrast are obtained by changing the gray-scale levels for the Amsler grid on the computer screen. The examination results obtained are then used to generate a 3-D map of the central visual field that shows the location, extent, slope, depth, and shape of any visual field defects present. 2.MethodsFor examination of a patient we use IBM-compatible personal computers with attached 17-inch touch-sensitive computer monitors. Each patient is positioned in front of the computer monitor. The angle of the visual field is determined by seating the patient at the fixed distance of 30 cm from the central fixation marker on the computer screen (0 deg horizontally and 0 deg vertically from fixation). An eye cover is used to completely cover the eye that is not being examined. Refractive correction is used with the patient’s contact lenses or eyeglasses when necessary. An Amsler grid at a preselected gray-scale level and preselected angular resolution is displayed by the computerized test program (Fig. 2). The patient is first asked to focus on a changing stimulus at the center of the grid. In order to suppress the central Troxler effect and keep the patient’s attention, the stimulus is regularly changed (by changing a set of characters, such as letters and numbers). The patient is asked to mark the areas on the Amsler grid that are missing from his or her field of vision by tracing this region with a finger on the touchscreen. Areas that are missing are defined as areas where the grid lines are distorted or missing. Increasing degrees of contrast are simulated by repeating this procedure at different gray-scale levels for the Amsler grid. The results are recorded and later displayed by the computerized test program after completion of the examination. An immediate 3-D depiction of the central 25 deg of the visual field (see Sec. 3) is obtained using these results. The third dimension is the retinal contrast sensitivity plotted as a function of retinal x-y position. The location, extent, slope, depth, and shape of the scotomas resulting from conditions affecting the (central) visual field can then be assessed. Each eye, depending on the patient’s compliance, requires a total of approximately 4 to 5 min to be tested. 3.ResultsIn several studies8 9 10 11 12 13 14 15 since the beginning of 2000, the 3-D computer-automated threshold Amsler grid test has proven to be successful for fast, accurate, noninvasive, and comprehensive visual field testing. The device has been in use since April 2000 at the Doheny Eye Institute in the Keck School of Medicine at the University of Southern California, and so far more than 200 patients have been examined or screened for glaucoma, age-related macular degeneration (AMD), optic neuritis, and anterior ischemic optic neuropathy (AION). In ocular hypertensive patients suspect for glaucoma, scotomas are difficult to detect by state-of-the-art standard automated perimetry,14 15 yet such visual field defects were repeatedly identified by the novel 3-D test, suggesting its effectiveness also as a screening tool.16 Example examination results for several ophthalmic disorders are shown in Fig. 3. The figure demonstrates some of the key features the new methodology provides. In Fig. 3(a) the 3-D plot of retinal contrast sensitivity as a function of visual field eccentricity exhibits a scalloped boundary of a visual field defect caused by optic neuropathy, with random islands of partial vision inside as opposed to a clean-cut steep cliff between vision and no vision in the case of anterior ischemic optic neuropathy that can be seen in Fig. 3(b).8 9 This feature lends itself to yet another criterion for distinguishing between these two diseases. Figure 33-D display of a visual field with a diagnosis of (a) optic neuropathy, (b) anterior ischemic optic neuropathy, (c) macular degeneration, and (d) glaucoma, recorded by the 3-D computer-automated threshold Amsler grid test. The x-y -axis denotes the horizontal and vertical coordinates of the visual field in degrees with (0,0) being the center of fixation. The z-axis denotes the contrast sensitivity of the retina expressed in percent. 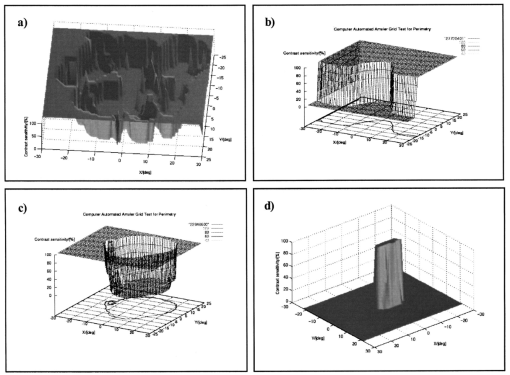 Figures 3(c) and 3(d) depict typical cases of age-related macular degeneration and advanced glaucoma. The 3-D depiction of visual field defects caused by these two diseases is both intuitive (AMD being a “central hole” and advanced glaucoma being a “confined mesa”) and informative. The 3-D depiction of the visual field defects can be further characterized by a slope along the circumference of the defects. The slope is defined as the percentage of loss in retinal contrast sensitivity over degrees of visual field. A steep slope would be representative of an absolute scotoma whereas a shallow slope would be indicative of a relative scotoma. 4.DiscussionWe have developed a 3-D computer-automated threshold Amsler grid testing technology with which we can determine the presence of visual field defects that are difficult to discern with more traditional testing methods. Furthermore, the high spatial resolution and three-dimensional aspects of this test permit a precise characterization of the nature and shape of these defects, which correlates with the underlying pathology. In short, this test has demonstrated greater sensitivity and reliability and higher resolution than traditional methods and, importantly, provides consideration of the third dimension, i.e. retinal contrast sensitivity. Furthermore, several diseases showed a characteristic signature pattern of visual field defects that is not obvious in two-dimensional assessments. For example, optic neuritis is depicted as a series of spires and valleys that probably reflect individual bundles of axons that became dysfunctional through demyelination or were alternately spared. In contradistinction, in anterior ischemic optic neuropathy, another disease of the optic nerve that sometimes is difficult to distinguish from optic neuritis, the topography was more of a plateau, with a sudden cliff reflecting the zone of infarct. Hence the consistent location, shape, and pattern of scotomas allow users of this test to make determinations very helpful in the differential diagnosis of a patient. The preliminary results of our study show great agreement between Humphrey visual field testing and the 3-D computer-automated threshold Amsler grid test.10 11 In 1982 Quigley and his colleagues demonstrated that despite the loss of more than 40 of the axons in the optic nerve (in glaucoma and other optic neuropathies), standard assessments of vision, including Snellen acuity and kinetic perimetry, most often remained normal. Some researchers have suggested that this reflects considerable “redundancy” in the human visual system. However, this begs the question, for redundancy seen another way actually reflects the insensitivity of our present instruments in the detection of visual abnormalities. In response to this, there has been a great increase of interest in testing sensory visual function. Known and novel approaches include brightness sense testing,17 critical flicker frequency,18 contrast sensitivity testing,19 electrophysiological tests of various sorts,20 threshold Amsler grid testing,6 and color vision testing in various forms of automated perimetry.21 While all of these methods provide new information, which taken as a whole is extremely useful in the characterization of visual impairments, there are realistic tradeoffs in time and other resources that make such extensive testing difficult, if not impossible. It is not uncommon for a patient to spend 8 h in a university eye department being subjected to all of these tests. This takes a considerable toll on patients, doctors, and insurance companies. The methodology described here provides many advantages over conventional perimetry and indeed other assessments of visual fields. It measures three dimensions rather than two in its depiction of scotomas, providing invaluable new insights into visual field defects. The new test has superior angular resolution. Generally we employ 1-deg grid spacing rather than the usual 6 deg employed by automated perimeters, which produces, at least in theory, a 36-fold higher spatial resolution. In short, this method provides a greater sensitivity, with unprecedented depiction of scotomas as 3-D structures, which assists in the detection and characterization of visual field defects. These quantitative and reproducible results also provide an excellent basis for monitoring the development of scotomas that are manifestations of a variety of diseases. While standard automotive perimetry tests are time-consuming, this new test is simple to use, patient friendly, and can be performed in 4 to 5 min per eye, making frequent testing more feasible.16 REFERENCES
R. P. Mills
,
“Automated perimetry. Part I,”
J. Am. Intraoc. Implant Soc. , 10 347
–353
(1984). Google Scholar
M. Amsler
,
“L’examen qualitatif de la fonction maculaire,”
Ophthalmologica , 144 248
–261
(1947). Google Scholar
M. Amsler
,
“Earliest symptoms of diseases of the macula,”
Br. J. Ophthamol. , 37 521
–537
(1955). Google Scholar
M. Wall
and
A. A. Sadun
,
“Threshold Amsler grid testing. Cross-polarizing lenses enhance yield,”
Arch. Ophthalmol. (Chicago) , 104
(4), 520
–523
(1986). Google Scholar
W. Fink
,
A. K. Hsieh
, and
A. A. Sadun
,
“Computer-automated 3D visual field testing in distinguishing paracentral scotomas of optic neuritis vs. AION,”
Invest. Ophthalmol. Visual Sci. , 41
(4), S311
(2000). Google Scholar
A. Fahimi
,
A. A. Sadun
, and
W. Fink
,
“Computer automated 3-D visual field testing of scotomas in glaucoma,”
Invest. Ophthalmol. Visual Sci. , 42
(4), S149
(2001). Google Scholar
P. P. Nazemi
,
W. Fink
,
J. I. Lim
, and
A. A. Sadun
,
“Paracentral scotomas of age-related macular degeneration detected by means of a novel computer-automated 3D visual field test,”
Invest. Ophthalmol. Visual Sci. , 42
(4), S705
(2001). Google Scholar
|
CITATIONS
Cited by 38 scholarly publications.
Visualization
Eye
Contrast sensitivity
Electrophysiological tests
Spatial resolution
3D displays
3D vision