|
|
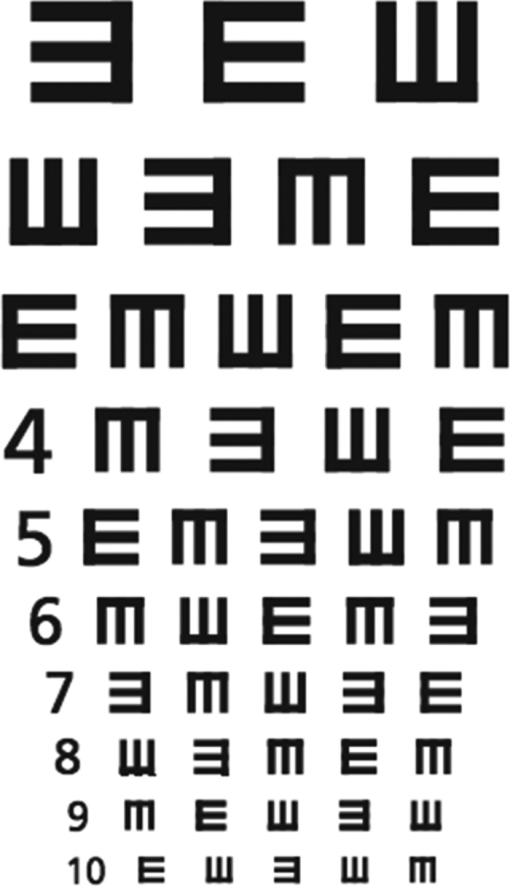
1.IntroductionThe conviction that visual acuity has an essential influence on the precision of manual work is well-known and widespread in many professions. Dentistry, with its small operating field and its demands for manual skills and precision, is particularly suited to the use of optical magnification. For decades, loupes have been used by dentists to improve precision,1, 2 as well as for ergonomic reasons.2, 3, 4, 5, 6, 7 Since the 1990s, the operating microscope has been promoted as a necessary part of dental equipment. Surprisingly, very little scientific research about the visual acuity of dentists, the influence of the different optical devices, and the relationship between visual acuity and precision in dental work has been published so far. An electronic search in the PubMed and Embase databases using the keywords “loupes,” “magnification,” or “visual acuity,” and their combinations yielded no more than 70 original articles, when endodontic publications were excluded and the search was limited to dental journals. The literature about optical magnification in dentistry is dominated by case reports and expert opinions that mostly praise the advantages of optical magnification),2, 6, 8, 9, 10 thus representing a body of evidence with the lowest possible evidence level. There is an obvious gap between the subjective conviction of the advantages of magnification for dental work and its scientific evidence. Burton and Bridgman11 examined the visual acuity of a group of dentists and dental students in New Zealand and showed a huge individual variability and also an influence of age on visual performance. Several other studies investigated the influence of age and showed a loss of accommodation (presbyopia) and low contrast sensitivity under testing conditions with low illumination with increasing age.8, 12, 13, 14, 15 Studies about loupes in restorative dentistry and adjacent tooth damage showed ambiguous results and suggest that the use of the tested magnification devices does not, per se, lead to better quality processes or results.1, 16, 17 Studies comparing the impact of different magnifications on diagnostic accuracy showed little18, 19 or no diagnostic gain.19 On the contrary, the use of loupes or clinical microscopes provokes an increase in false positive results, despite an increase in sensitivity.20, 21 Loupes are classified according to their different optical construction into single lens loupes, Galilean loupes, and Keplerian loupes. Dependent on the optical construction, different magnification factors are possible. A typical magnification factor for Galilean loupes is 2.5× with an upper limit of 3.2×. Keplerian loupes allow a free choice of the magnification factor. However, due to practical reasons, it is commonly between 3.5× and 4.5×. The diversity of loupe systems, the variability in natural visual acuity, and the influence of age and adjustments suggest that the impact of loupes on dental treatment quality might be more complex than expected. The aim of the present study was to evaluate with a new visual test the effect of different magnification devices on the near visual acuity of a group of dentists and to analyze how this effect is influenced by the dentist's age and natural visual acuity. 2.Materials and MethodsForty dentists from the Dental School of Bern, Switzerland, were enrolled in the testing procedure (age distribution, Table 1). Miniaturized visual tests with E-optotypes, well-known to opticians, allowed a test of the visual acuity at a typical dental working distance (Fig. 1). The miniaturization of these tests was achieved by precision pictures on diapositive films (Kodachrome 64, KODAK, Rochester, New York). The dimension of the E-optotypes ranged from 0.05 to 0.58 mm. The transparent tests were fixed behind a fenestrated black cardboard (0.5 mm) and mounted on a negatoscope. Table 1Age distribution of participating dentists.
The visual test was carried out under four different conditions, whereby the negatoscope was at eye-level and the chin could be supported on the hands. There was no special training with the different loupe systems.
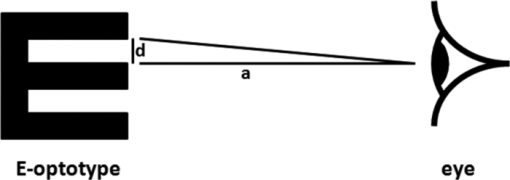
The loupes were mounted to a headband, allowing the wearing of individual eyeglasses in all groups. During all visual tests, the position of the loupes, the eye-object-distance, and the reading of the E-optotypes were supervised by the same expert. The smallest line that could be read without mistakes was registered. The values of the recorded lines of the E-optotypes were converted in visual acuity units by the following formula: Visual acuity = 1/angular visual acuity. The angular visual acuity is defined as the smallest angle, in minutes, under which two adjacent points can be separately recognized. In the visual tests, these points are two adjacent arbors of the E (= 1/5 the size of E). First, the angle epsilon (ɛ) had to be calculated with the formula 1. ɛ = tan−1(d/a), and then the visual acuity was calculated according to the formula 2. visual acuity = 1/(ɛ×60) (Fig. 2).22, 23 For part 1 of the study, the influence of the different magnification systems on the visual acuity was investigated for all tested dentists. In part 2, the same dentists were divided into two subgroups: group A included those with age<40 years and group B included those with age ≥ 40 years. The age cut-off of 40 years was chosen because literature reports this to be the age at which natural changes in the eye begin.13, 14 For part 3, the dentists were classified by their natural visual acuity as assessed in part 1: group C presented a natural visual acuity of 1.1 or more and group D presented a value <1.1. The cut-off value of 1.1 was chosen according to the test results with the aim to obtain two evenly divided groups. For statistical analysis, the software SAS 9.1.3 (SAS Institute Inc., Cary, North Carolina) was used. The significance level was set at α = 0.05. Descriptive statistical analysis was carried out to determine the means and medians as well as the nonparametrical 95% confidence intervals (CIs) for all dentists and for the subgroups A to D. The influence of the respective groups of dentists and different loupe systems on the visual acuity was analyzed using two nonparametric repeated measures ANOVA models, namely F1_LD_F1 models after Brunner, Domhof, and Langer,24 followed by Wilcoxon Mann Whitney tests and Wilcoxon signed rank tests with Bonferroni–Holm correction for multiple comparisons as post-hoc tests. 3.ResultsThe mean visual acuities, medians, and 95% CIs for all tested dentists are presented in Table 2. The highest visual acuity was obtained with the Keplerian system, followed by the Galilean system, the single lens loupe, and finally, the natural visual acuity. Statistical analysis revealed significant differences between all tested conditions (p<0.001) (Table 2). Table 2Visual acuities for all tested dentists under different magnification conditions: Natural vision in a working distance of 300 mm (NV) showed a huge interindividual variability. Single lens (S), Galilean (G), and Keplerian (K) loupes showed an improvement dependent on their magnification factor. Within the columns, significant differences are represented by the superscript letter (a: p<0.001).
The mean visual acuities, medians, and 95% CI for groups A and B (< and ≥40 years, respectively) are presented in Table 3. There was a moderate correlation between the participants’ age and their visual acuity (Cohen's kappa 0.53). For all tested conditions, significant differences between the two groups were detected. Both groups profited from magnification of the single lens loupe and even more from the sophisticated optics of the Galilean and Keplerian loupe (Table 3). Table 3Visual acuities for the groups <40 and ≥40 years under different magnification conditions: natural visual acuity (NV), single lens loupe (S), Galilean system (G), and Keplerian system (K). Within the columns, significant differences are represented by the superscript letter (a: p<0.05).
The mean visual acuities, medians, and 95% CI for the groups C and D (natural visual acuity ≥1.1 and <1.1, respectively) are presented in Table 4. Statistical analysis detected significant differences between groups C and D for all tested conditions. Without magnification, group C achieved significantly better visual acuity than group D (p<0.001); this was also true when using the single lens loupe (p<0.001), the Galilean loupe (p<0.001), and the Keplerian loupe (p<0.01) (Table 4). Group C showed a significantly higher visual acuity without magnification than did group D with the help of a single lens loupe (p<0.01), but a lower visual acuity than was found in group D assisted by a Galilean or Keplerian loupe (p<0.0001). Table 4Visual acuities for the groups with a natural visual acuity ≥1.1 and <1.1 under different magnification conditions: natural visual acuity (NV), single lens loupe (S), Galilean system (G), and Keplerian system (K). Within the columns, significant differences are represented by the different superscript letters (a: p<0.001, b: p<0.05).
4.DiscussionThe body of evidence for using magnification devices in dentistry is weak: in particular, near vision in the dental working distance has rarely been tested. This might be due to the fact that the tests commonly used for near vision, such as the reading type test of the British Faculty of Ophthalmologists, are obviously not sensitive enough for dental purposes, and a commonly accepted visual test that would fulfill the necessary optical requirements is not available. Near vision, as assessed by the above-mentioned reading type test, was assessed in a group of dentists and showed adequate near visual acuity in 93.5%,15 99.91%,25 and 100%.26 This test is composed of passages of text at known type-face sizes from N5 upward. N5 is a historic dimension unit that is equivalent to 0.9 mm for lower case letters in Times Roman.27 If almost all of the test subjects can read the smallest line, then this test seems to be inadequate for dental purposes. A comparison of N5 with the range of E-sizes used in this study could support this conclusion. Only one study used miniaturized Snellen tests, which do show the variability in dentist's natural near vision.11 Snellen charts are well-known from optician's acuity tests and consist of randomly arranged letters in downsizing lines. This test allows an objective acuity measurement but has the disadvantage that some letters are easier to recognize than others. Only tests with E-optotypes or Landolt-Rings allow a more objective measurement of visual acuity and the calculation of the vision angle. For the present study, E-optotypes ranging from 0.05 to 0.58 mm were chosen. As 39 out of 40 participating dentists were able to read the biggest line without magnification aids, and as all of them failed to read the smallest line even when using the biggest magnification factor, we consider the selected test size to be adequate. The miniaturization of these tests in an adequate and precise dimension was one of the challenges of this study. In summary, the use of a miniaturized common and validated test in the chosen dimensions seems to be adequate to measure near visual acuity for dental purposes. The aim of a further study should be the comparison of this miniaturized test with the common test applied by an optician. As shown by the results, the natural visual acuity varies highly between individuals. Dentists may compensate for visual deficiencies by using different magnification devices, such as the tested loupes. Even a single lens loupe leads to better visual performance, but the small, physically-determined working distance of 250 mm is ergonomically compromising. Therefore, single lens loupes are not normally recommended because of their inappropriate ergonomics and optical aberrations.6, 28 Nevertheless, this optical system was tested as it is still a common magnification device in dental practice thanks to its light weight and low cost. Improved optics such as the Galilean and Keplerian loupes, are more convenient as they allow an individualization of the working distance and, in part, the magnification factor. The tested Galilean system was chosen as a reference of Galilean systems, with the common magnification of 2.5× and the possibility of attachment to a headband that allows for the wearing of glasses. This system enabled improved visual acuity at the typical working distance for dentists. In previous publications, Galilean loupes have been especially recommended for dental students, dental hygienists, and periodontists and as a good entry point for those unfamiliar with magnification.8, 28 In the present study, the Keplerian loupe with a magnification of 4.3× achieved the best visual acuity at the typical working distance for dentists. This is mainly due to the higher magnification factor, but perhaps also to the absence of chromatic and optical aberrations. A direct comparison between a Galilean and a Keplerian system with the same magnification factor was not possible because Keplerian loupes with 2.5× are not on the market because of their heavier weight and more complicated construction. However, the significant difference between the tested Galilean and Keplerian loupe is remarkable. This result indicates that in studies of loupes, the choice of the tested loupe system is important. Many previous studies have reported presbyopia and a loss of visual acuity with increasing age. This was confirmed in the present study, as a lower natural visual acuity was found for the older dentists (≥40 years), which may be due to changes in the eye that begin at this age.13, 14 Dentists suffering from presbyopia can compensate for their visual deficiencies by using magnification devices, but they may not achieve the visual acuity that they had at a younger age. The younger dentists in this study obtained significantly higher visual acuity than did the older dentists, independent of the tested magnification device. The Keplerian loupe even showed the highest differences between the two age groups, which may be due to the complexity of this optical system. With increasing magnification, the depth of the field becomes smaller, allowing fewer tremors of the hand or head, which might be more difficult for older dentists. Moreover, the lower contrast sensitivity that was reported for older dentists (>40 years) may be a factor that negatively influences the visual acuity, especially with a decreasing size of the E-optotypes).12, 14 Another reason for the high difference between the older and the younger group of dentists with Keplerian loupes may be the fact that younger people are more adaptive, allowing them to handle a complex loupe system more easily. In part 3 of this study, the dentists were classified according to their natural visual acuity (</≥1.1) to determine if both groups benefited in the same degree from magnification devices, what could be confirmed in this study. Nevertheless, it is apparent that there are individuals that can achieve a higher acuity without any magnification than others with the assistance of the Galilean loupe. Only when using the Keplerian loupe did all dentists achieve a higher visual acuity than anyone did with natural vision. 5.ConclusionMagnification devices, the dentist's age, and their natural visual acuity all have a significant influence on visual performance in the dental working distance. Dentists should be aware of their own visual performance and of the methods available to compensate their visual deficiencies. Magnification devices are recommended for dentists with low natural visual acuity and for dentists with good visual acuity. By using magnification aids such as Galilean or Keplerian loupes, dentists with low natural visual acuity can see better than can dentists with high natural visual acuity without magnification aids. AcknowledgmentsThe authors thank Philippe Ducreux (Lunea-Group, France), Professor Andreas Ettemeyer (NTB Interstaatliche Hochschule für Technik Buchs, Buchs, Switzerland), Martin Roost (Roost-Optik, Schaffhausen, Switzerland), and René Seiler (Fischer & Loeliger Optik, Bern, Switzerland) for their support with optical issues. The authors also thank Stefanie Hayoz (Institute of Mathematical Statistics, University of Bern, Switzerland) for the statistical analysis. ReferencesD. C. van Gogswaardt,
“Dental treatment methods using the loupe,”
ZWR, 99
(8), 614
–617
(1990). Google Scholar
M. J. Friedman,
“Magnification in a restorative dental practice: from loupes to microscopes,”
Compend. Contin. Educ. Dent., 25
(1), 53
–45
(2004). Google Scholar
S. Sunell and
L. Rucker,
“Surgical magnification in dental hygiene practice,”
Int. J. Dent. Hyg., 2
(1), 26
–35
(2004). https://doi.org/10.1111/j.1601-5037.2004.00061.x Google Scholar
M. S. Hagge,
“Use of surgical telescopes by senior dental students: a survey,”
J. Prosthodont., 12
(4), 271
–279
(2003). https://doi.org/10.1016/S1059-941X(03)00103-7 Google Scholar
J. P. Maillet, A. M. Millar, J. M. Burke, M. A. Maillet, W. A. Maillet, and
N. R. Neish,
“Effect of magnification loupes on dental hygiene student posture,”
J. Dent. Educ., 72
(1), 33
–44
(2008). Google Scholar
S. E. Syme, J. L. Fried, and
H. E. Strassler,
“Enhanced visualization using magnification systems,”
J. Dent. Hyg., 71
(5), 202
–206
(1997). Google Scholar
N. U. Zitzmann, M. D. Chen, and
R. Zenhausern,
“Frequency and manifestations of back pain in the dental profession,”
Schweiz Monatsschr Zahnmed, 118
(7), 610
–618
(2008). Google Scholar
B. J. Millar,
“Focus on loupes,”
Br. Dent. J., 185
(10), 504
–508
(1998). https://doi.org/10.1038/sj.bdj.4809853 Google Scholar
P. Perrin, D. Jacky, and
P. Hotz,
“The operating microscope in dental general practice,”
Schweiz Monatsschr Zahnmed, 110
(9), 946
–960
(2000). Google Scholar
A. H. Forgie,
“Magnification: what is available, and will it aid your clinical practice,”
Dent. Update, 28
(3), 125
–128
(2001). Google Scholar
J. F. Burton and
G. F. Bridgman,
“Presbyopia and the dentist: the effect of age on clinical vision,”
Int. Dent. J., 40
(5), 303
–312
(1990). Google Scholar
A. J. Adams, L. S. Wong, L. Wong, and
B. Gould,
“Visual acuity changes with age: some new perspectives,”
Am. J. Optom. Physiol. Opt., 65
(5), 403
–406
(1988). Google Scholar
J. A. Gilbert,
“The dentist and the aging eye,”
J. Mo. Dent. Assoc., 60
(3), 22
–24
(1980). Google Scholar
G. C. Woo and
B. Ing,
“Magnification devices for the presbyopic dentist,”
J. Can. Dent. Assoc., 54
(6), 447
–449
(1988). Google Scholar
A. H. Forgie, T. Gearie, C. M. Pine, and
N. B. Pitts,
“Visual standards in a sample of dentists working within Scotland,”
Prim. Dent. Care, 8
(3), 124
–127
(2001). https://doi.org/10.1308/135576101322561976 Google Scholar
A. Lussi, O. Kronenberg, and
B. Megert,
“The effect of magnification on the iatrogenic damage to adjacent tooth surfaces during class II preparation,”
J. Dent., 31
(4), 291
–296
(2003). https://doi.org/10.1016/S0300-5712(03)00029-0 Google Scholar
B. Zaugg, A. Stassinakis, and
P. Hotz,
“Influence of magnification tools on the recognition of simulated preparation and filling errors,”
Schweiz Monatsschr Zahnmed, 114
(9), 890
–896
(2004). Google Scholar
H. Erten, M. B. Uctasli, Z. Z. Akarslan, O. Uzun, and
E. Baspinar,
“The assessment of unaided visual examination, intraoral camera and operating microscope for the detection of occlusal caries lesions,”
Oper. Dent., 30
(2), 190
–194
(2005). Google Scholar
A. Lussi,
“Comparison of different methods for the diagnosis of fissure caries without cavitation,”
Caries Res., 27
(5), 409
–416
(1993). https://doi.org/10.1159/000261572 Google Scholar
F. M. Mendes, E. Ganzerla, A. F. Nunes, A. V. Puig, and
J. C. Imparato,
“Use of high-powered magnification to detect occlusal caries in primary teeth,”
Am. J. Dent., 19
(1), 19
–22
(2006). Google Scholar
R. Haak, M. J. Wicht, M. Hellmich, A. Gossmann, and
M. J. Noack,
“The validity of proximal caries detection using magnifying visual aids,”
Caries Res., 36
(4), 249
–255
(2002). https://doi.org/10.1159/000063926 Google Scholar
E. Hecht, Optik, Oldenbourg Wissenschaftsverlag, München
(2005). Google Scholar
J. Trotter, Das Auge: Ein Handbuch für Augenoptiker, Optik Verlag Trimbach, Switzerland
(1995). Google Scholar
E. D. S. L. Brunner, Frank, Nonparametric Analysis of Longitudinal Data in Factorial Experiments, Wiley, New York
(2002). Google Scholar
A. Rawlinson,
“A study to investigate the visual quality of dental undergraduates using a simple screening programme,”
Aust. Dent. J., 33
(4), 303
–307
(1988). https://doi.org/10.1111/j.1834-7819.1988.tb04182.x Google Scholar
A. Rawlinson,
“A simple eyesight screening programme for dental undergraduates: results after 7 years,”
Aust. Dent. J., 38
(5), 394
–399
(1993). https://doi.org/10.1111/j.1834-7819.1993.tb05522.x Google Scholar
A. Hedin,
“Aviation Ophthalmology,”
(2006) Google Scholar
M. A. Mansueto and
J. D. Overton,
“A clinician's guide to purchasing surgical loupes,”
Tex. Dent. J., 124
(2), 174
–186
(2007). Google Scholar
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||