|
|
1.IntroductionPhotodynamic therapy (PDT) uses a photosensitizer or a photoactivated dye in combination with a visible light that produces a reactive oxygen species and destroys both tumor cells and malignant tissue.1 The PDT efficacy depends on the light excitation energy distribution, photosensitizer concentration, and oxygen transport and consumption during the treatment. However, conventional PDT does not consider the laser irradiation dose during PDT. For the optimization of treatment planning, it is essential to know how light is transported within the tissue. Using knowledge of the optical properties (absorption coefficient μ a [mm−1] and reduced scattering coefficient μ ′ s [mm−1], etc.) of the target tissue, the light distribution and propagation within the tissue can be estimated.2 The change of optical properties by laser treatments is particularly interesting. The light propagation within the tissue changes according to the change of optical properties in laser irradiation.3, 4 Recently, the optical properties of various normal and pathologic tissues have been determined at a single wavelength or over a broad wavelength range. However, there is little information about the change of the optical properties of tissues by PDT in the wide wavelength range.5, 6, 7, 8 The light fluence rate in tissue, by determining the optical properties of PDT-treated tissue, in PDT realizes a pre-estimated and safe treatment effect. The objective of this study is to determine the optical properties of tissues, which are treated by PDT in the wavelength range from 350 to 1000 nm. In this study, the mouse tumor model that inoculated Lewis lung carcinoma (LLC) cells was used to perform PDT-treatment on tumor tissue. The optical properties of tissues were determined by using the double integrating sphere measurement system9, 10, 11, 12, 13 combined with the inverse Monte Carlo method.11, 12, 13, 14, 15, 16 This paper presents the determination of the optical properties of mouse tumor tissues during and after PDT in vitro, and the optical penetration depth of the tumor tissue. 2.Material and Methods2.1.Animals Model and Sample PreparationNineteen syngeneic male C57BL/6 mice at six weeks of age were used. The LLC cells were maintained at 37°C and 5% CO2 in Dulbecco's Modified Eagle's Medium (Sigma-Aldrich Inc., USA) containing 10% fetal calf serum (BioWest Inc., France), 100 units/mL penicillin, and 0.1 mg/mL streptomycin (Nacalai Tesque Inc., Japan). Cells were prepared at 1 × 107 cells/mL for injection. All animals received subcutaneous bolus injections of 0.1 mL of cell suspension in the lower dorsal region using a 23-gauge needle. Each tumor was grown for seven days. Tumor diameter was reached about 11.5 mm on average. For optical property measurement of tissues, the animals were euthanized by an overdose of anesthesia. The tumor tissues were resected using a surgical knife. Then, the skin and the scab of the tissue were removed. The sample was approximately 2 mm in thickness except the sample that was obtained seven days after treatment. The sample thickness of the tissue obtained seven days after treatment was 1 mm due to the removed sample was 1 mm in thickness. Each section was positioned between slide glasses. The optical properties of the tissue were measured with the double integrating sphere setup within 30 min after sacrifice. The animal experimentation was carried out according to the guideline of animal experimentation of Osaka University. 2.2.PDT TreatmentAs a photosensitizer, talaporfin sodium (Laserphyrin®, MEIJI SEIKA KAISHA, Japan)17 was used. 16 tumor-bearing mice were intravenously injected with talaporfin sodium. While the remaining four were control groups without injection. Before injection, talaporfin sodium was reconstituted in the physiological saline and used at a concentration of 5 mg/kg body weight. Talaporfin sodium was injected via the tail vein two hours prior to light exposure. The tumor surface was irradiated superficially through the skin with a laser diode emitting continuous wave laser light at a wavelength of 664 nm (UM1000 Dental_665, JENOPTIK unique-mode GmbH, Germany).18 The light was collimated with a lens, and the spot diameter was 12.5 mm. The animals were chosen at random to populate. Table 1 summarizes the treatment conditions. For determination of the tumor tissue optical properties during PDT, the irradiation was performed 1 min to five mice before each measurement of the optical property. And, the light irradiation of 5 min was carried out to five mice. The average power density on the tumor surface was 100 mW/cm2. For determination of the tissue optical properties after PDT, each tumor of six mice were irradiated with a light dose of 100 J/cm2. The average power density on the tumor surface was 100 mW/cm2. During light irradiation, individual animals were restrained un-anesthetized in holders. Then, 1, 2, and 7 days after PDT the tumor tissue was resected and the tissue optical properties were measured. Fig. 7Optical penetration depth of PDT-treated tumor tissues. (a) Optical penetration depth of tumor tissues during PDT. (b) Optical penetration depth of tumor tissues after PDT. 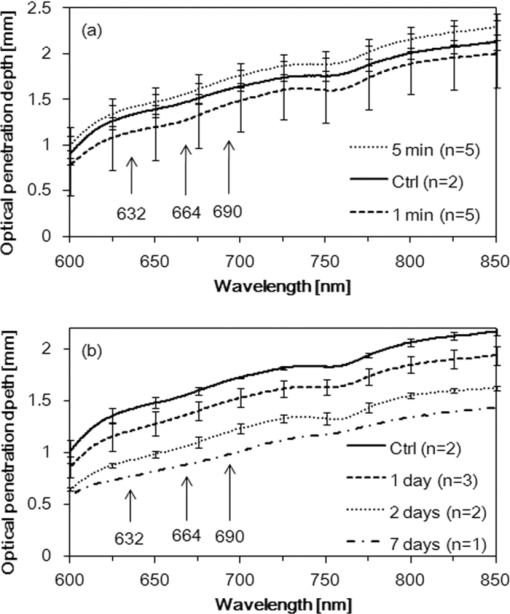 Table 1Experimental conditions of PDT.
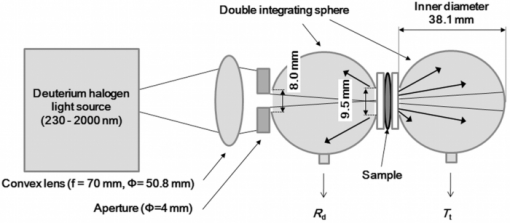
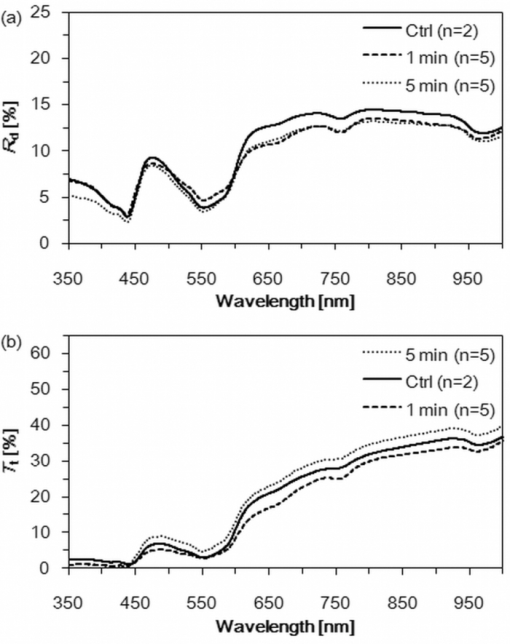
2.3.Double Integrating Sphere SetupA double integrating sphere system was designed for the measurement of optical properties of biological tissues. This is also a convenient tool since it simultaneously measures diffuse reflectance (R d) and total transmittance (T t). Using an integrating sphere as both a diffuse illumination source and a detector provides a technically simple measurement apparatus. The experimental setup is presented in Fig. 1. Balanced deuterium tungsten halogen source (DH-2000-BAL, Ocean Optics, USA) combined with high-powered halogen light source (HL-2000-HP, Ocean Optics, USA) were employed as a light source. Specimens were placed between two integrating spheres (FOIS-1, Ocean Optics, USA). The integrating sphere was 38.1 mm inner diameter. The inside surface of the sphere was coated with diffusely reflective material, SpectralonTM. The entrance port size of the reflectance sphere was 8.0 mm in diameter and the sample port of both spheres was 9.5 mm in diameter. The beam-illuminated area was 3 mm in diameter on the sample. The incident light was diffusely reflected from the sample surface and the light was diffusely transmitted during the sample. Then, the reflected and transmission light were multiply scattered in spheres and recorded by spectrophotometer (Maya2000 Pro, Ocean Optics, USA) as R d and T t, respectively. From these experimental data, the set of optical properties were calculated using the inverse Monte Carlo technique. 2.4.Inverse Monte Carlo MethodThe inverse Monte Carlo technique was employed to calculate the optical properties of samples from measured values of R d and T t. Calculation of the tissue optical properties was performed at each wavelength point. The algorithm consists of following steps: a. To calculate the optical parameters (R d and T t) with Monte Carlo simulations, which was developed by Wang,2 an initial set of optical properties had been estimated. b. The Monte Carlo simulation was performed on this initial set of data. c. A simulated set of the optical parameters was compared to the actual measurements. If agreement between calculated and measured data was within a defined error limit (<0.5%), the set of optical parameters was accepted for the sample. d. This procedure was repeated with a new set of optical properties until the error threshold was achieved. With this iterative process, the set of optical properties that yields the closest match to the measured values of reflectance and transmittance are taken as optical properties of the tissue. This method allows one to determine the μ a and μ s of a tissue from the measured values. Then, the μ ′ s was calculated by Eq. 1[TeX:] \documentclass[12pt]{minimal}\begin{document}\begin{equation} \mu _s ' = \mu _s \left({1 - g} \right), \end{equation}\end{document}2.5.Histological StudyTumors were harvested after PDT and fixed in 8% buffered formalin. The tumors were then embedded in paraffin and stained by hematoxylin and eosin. 2.6.Statistical AnalysisA student's t-test was used to evaluate the significance of the difference between obtained optical properties of tumor tissues. The differences between optical coefficients of control and PDT-treated tissues were considered to be statistically significant when the calculated probability valued (p value) was equal or less than 0.05. P value ≤ 0.05 means that the probability that the two data sets are different is ≥ 95%. This level of significance is considered acceptable for the biological samples. 3.Results3.1.Macroscopic Observations of Photodynamic Therapy EffectThe tumor tissues after 1 and 5 min of irradiation did not show significant changes as shown in Figs. 2b and 2d. However, the PDT-treated tumors showed changes 1, 2, and 7 days after PDT as shown in Figs. 2f, 2g, 2h. After PDT, a tumor showed a dusky black discoloration. Fig. 2Photograph of tumor tissues during and after PDT. (a) Gross lesion of tissue before PDT. (b) Tumor tissue after irradiation of 100 mW/cm2 for 1 min. (c) Gross lesion of untreated tissue. (d) PDT-treated tissue after completion of irradiation of 100 mW/cm2 for 5 min. (e) Tumor tissue before PDT. (f) One day after PDT. Laser irradiation was performed with 100 mW/cm2 for 1000 s. (g) Two days after PDT. Tumor was irradiated with 100 mW/cm2 for 1000 s. (h) Seven days after PDT. Tumor was irradiated with 100 mW/cm2 for 1000 s. 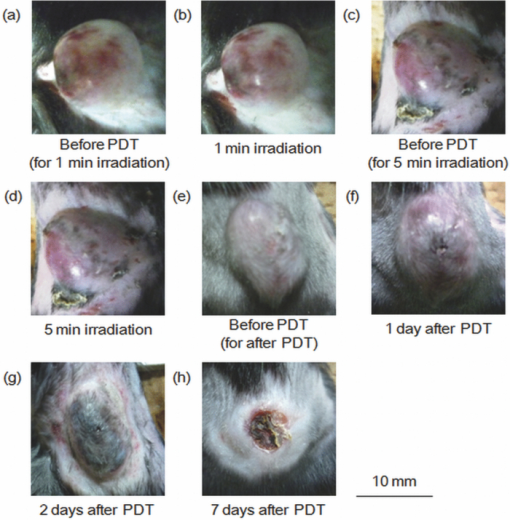 3.2.Tumor Tissue Optical Properties during Photodynamic TherapyOptical properties were calculated from the experimental measurements of R d and T t of 1 and 5 min irradiated tumor tissues for the determination of the optical property of the tumor tissue during PDT. The R d and T t spectra of the tumor tissues are shown in Figs. 3a and 3b, respectively. The μ a and μ ′ s spectra of tumor tissues were shown in Figs. 4a and 4b, respectively. There were several peaks in the μ a spectra as shown in Fig. 4a. For tumor tissues before PDT, the peaks were at 439 and 553 nm with mean μ a values of 1.18 and 0.77 mm−1, respectively. These peaks corresponded to the absorption of the hemoglobin.22 Scattering, depicted in Fig. 4b, was greater at shorter wavelength with a peak value of about 1.52 mm−1 at the wavelength of 350 nm and smoothly declined over the visible range to a level of about 0.41 mm−1 at the wavelength of 1000 nm. During PDT, the μ a and μ ′ s spectra were not changed. 3.3.Tumor Tissue Optical Properties after Photodynamic TherapyThe μ a and μ ′ s spectra of the tumor tissues 1, 2, and 7 days after PDT are shown in Figs. 5a and 5b, respectively. A considerable difference of the mouse tumor tissue optical properties, before and after PDT, was observed. Table 2 summarizes optical properties changes observed in PDT-treated tumor tissues compared with before-treatment tissues in a specific region for PDT-treatment from 600 to 700 nm for the individual wavelengths, such as 632, 664, and 690 nm. After PDT, the values of μ ′ s increased with the passage of time as shown in Fig. 5b. Table 2Tumor tissue optical properties during and after PDT.
4.Discussion4.1.Histological AnalysisIt seems clear that a significant increase of μ ′ s should be a result of substantial structural changes. As shown in Fig. 6, corresponding changes of mouse tumor tissue structures after PDT were revealed by a histological evaluation of the tumor samples and were compared to sections from non-PDT treated tissue. A histological analysis has shown that PDT causes the blood vessel disruption and leak of erythrocytes [Fig. 6e]. Our histological findings confirm the results obtained by Nelson 23 for mouse tumor tissues. It has been shown that specific phenomena, such as microvascular disruption, occur after the completion of PDT. Furthermore, a leak of erythrocytes is caused by vascular damage. A mouse's red blood cell size is about 6 μm in diameter.24 Blood is a scattering system that consists of scattering particles, such as red blood cells, their aggregates, and the surrounding media (i.e., plasma). The refractive index mismatching between red blood cells cytoplasm and blood plasma is the major source of light scattering in blood.25 The scattering properties of blood are dependent on RBC volume.11 As a result, the concentration of chromophores and scattering inhomogeneities increases and tissues become optically denser, which likely leads to a significant increase of μ ′ s in the spectral range from 600 to 1000 nm. Seven days after PDT, the PDT-treated tissues showed the decrease of tumor cells and fibrosis as shown in Fig. 6f. This pathological change has been observed in the clinical treatment26 and μ ′ s of the tissue increased as shown in Fig. 5b. Saidi found that the large collagen fibers of the dermis were primarily responsible for the light scattering in the skin.27 They indicated that scattering of normally incident light by a single fiber, as predicted by the Mie theory, was dependent on the wavelength of the indices of refraction of the fibers and of the surrounding medium. Perhaps, the collagen fibers shown in the PDT-treated tissue played a role of the scatter in the tissue. Then, the μ ′ s of the treated tissue measured seven days after treatment increased. Fig. 6H&E staining of tumor tissues. (a) and (d) show the Lewis lung carcinoma tissue before PDT. Tumor microvessels are shown. (b) and (e) show the tumor tissues 1 day after PDT. The blood vessel damage and leak of erythrocyte are shown after PDT. (c) and (f) show the PDT treated tumor tissue seven days after PDT. Decrease of tumor cells has been observed. The PDT treated tissue has shown fibrosis. 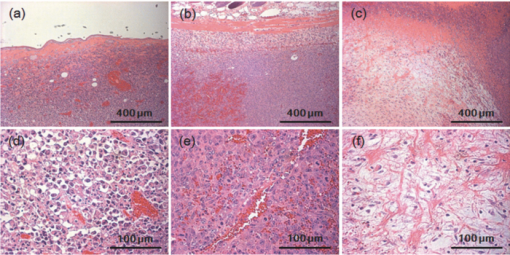 4.2.Penetration Depth of Light within Tumor Tissues during Photodynamic TherapyThe penetration depth of light into a biological tissue is an important parameter for the correct determination of the irradiation dose in the PDT of various diseases. The estimation of the light penetration depth was performed with Eq. 2 (Ref. 28) Eq. 2[TeX:] \documentclass[12pt]{minimal}\begin{document}\begin{equation} \sqrt {{1 / {3\mu _a \big(\mu _a + \mu _s '\big)}}}. \end{equation}\end{document}The optical penetration depth of tumor tissues during PDT was calculated with the calculated optical properties presented in Fig. 4 and the results are presented in Fig. 7a. The optical penetration depth of the tumor tissues after PDT was calculated with the optical properties presented in Fig. 5 and the result is presented in Fig. 7b. Table 3 summarizes the optical penetration depth changes observed in PDT-treated tumor tissues compared with before-treatment tissues in a specific region for PDT-treatment from 600 to 700 nm for the individual wavelengths, such as 632, 664, and 690 nm. Comparison of the tumor tissue optical properties before PDT obtained in this study and those presented by Bargo 29 shows an agreement between them. The μ a and μ ′ s spectra of the sample are qualitatively similar to the reported spectra in the spectral range from 600 to 900 nm. Literature values29 for in vivo optical properties of human lung tumor tissues at the wavelength of 630 nm have μ a ranging from 0.097 to 0.488 mm−1 and μ ′ s ranging from 0.63 to 1.15 mm−1, which are in agreement with the results obtained in this study. Fig. 4Absorption coefficient μ a spectra and reduced scattering coefficient μ ′ s spectra of tumor tissues during PDT. (a) μ a spectra of tumor tissues performed 1 and 5 min irradiation. (b) μ ′ s spectra of the tumor tissues. 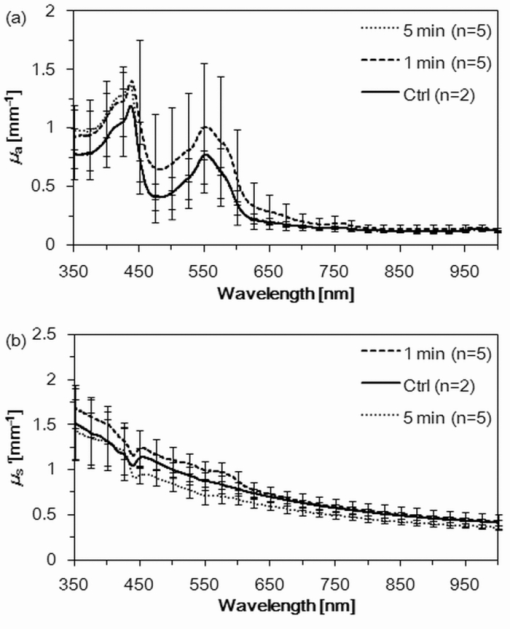 Fig. 5Absorption coefficient μ a spectra and reduced scattering coefficient μ ′ s spectra of tumor tissues during PDT. (a) μ a spectra of tumor tissues 1, 2, and 7 days after PDT. (b) μ ′ s spectra of the tumor tissues. 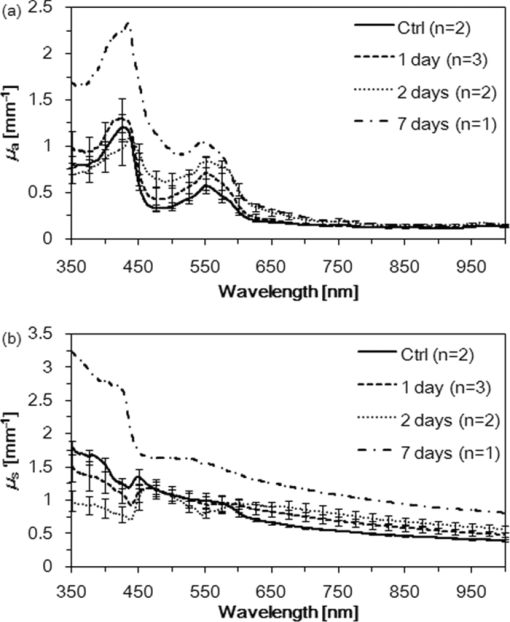 Table 3Optical penetration depth of tumor tissues during and after PDT.
During PDT, the penetration depth of light was not changed. Recently, the optical properties of in vivo human prostate during motexafin lutetium-medicated photodynamic therapy has been presented by Zhu for the wavelength 732 nm.8 For the wavelength, the effective attenuation coefficient varied after PDT, although the magnitude of the change was generally much smaller. The inverse of the effective attenuation coefficient gives us an estimation of the penetration depth. These results are compatible with our results on the optical penetration depth obtained in this study. Swartling researched the interstitial PDT with online feedback to deliver a tailored light fluence dose, exceeding a predefined threshold dose, to the whole prostate gland and adapt the dose plan in cases where the optical attenuation changes during the therapy.30 They have reported that the optical properties of the gland tissue did not markedly vary during the treatment with Foscan® in clinical study. But, Thompson reported that light transmission decreased in nodular basal cell carcinomas during 5-amino levulinic acid mediated PDT.31 They discuss that the light transmission changes are in fact due to the tissue oxygenation and changes in blood volume. Therefore, a system for interactively controlling the treatment to achieve the optimal therapy adapted for each case is needed in light dosimetry during PDT. After PDT, the penetration depth decreased with the passage of time as shown in Table 3. Compared to the tissue obtained before the treatment, the optical penetration depth of the tissue seven days after PDT decreased by 1.4 to 1.8 times. In general, if the cancer was not cured after the first PDT-treatment, a second treatment was carried out in PDT.32 In this study, we found the fact that the optical properties of PDT-treated tumor were changed. As a result, the light penetration depth of the mouse tumor tissues decreased after PDT. For precisely conducting the re-irradiation of PDT, the irradiation dose might be determined based on the optical properties of the PDT-treated tissues. The PDT-treated tissue optical properties will continue to be studied until a complete recovery is obtained and will be presented in future work. It is difficult to accurately estimate the experimental error in a study of this type in which many independent measurements are conducted. Experimental contributions to the error included the inaccuracy of the spectrometer, which we estimate to be <1% of the corresponding 100% value. This error becomes more prominent as the measured values of R d and T t become smaller, such as in the wavelength between 350 nm to 600 nm. Furthermore, there is a significant biological variability between the samples. For example, if the blood of the samples varied, this would be particularly noticeable in the wavelength range between 350 to 600 nm. This may have introduced an error in the μ ′ s spectra as shown in Figs. 4b and 5b. 5.ConclusionThe change of the optical properties of mouse tumor tissues by PDT in the wavelength range from 350 to 1000 nm were measured with the double integrating sphere system and the inverse Monte Carlo technique. No significant change could be detected during PDT. The optical property of the tumor tissue dramatically changed after PDT. Especially, the μ ′ s increased after PDT. After PDT-treatment, resulting in the change of mouse tumor tissue optical property, the light penetration depth into the tumor tissue decreased with the passage of time. To ensure the effective treatment procedure, an adjustment of the laser parameter in view of the decreasing penetration depth is recommended for the re-irradiation PDT. These tissue parameters become available for more models to predict optical distributions in tissues. The optical property obtained in vitro using the combination of double integrating sphere measurements and an inverse Monte Carlo technique are clearly useful for in vivo applications. AcknowledgmentsThis development was supported by SENTAN, JST. The authors wish to acknowledge the assistance of Yuki Nakata. They express their appreciation to Toshihiro Kushibiki for his helpful suggestions. ReferencesA. P. Castano, T. N. Demidova, and
M. R. Hamblin,
“Mechanisms in photodynamic therapy: part three-photosensitizer pharmacokinetics, biodistribution, tumor localization and modes of tumor destruction,”
Photodiagnosis Photodyn. Ther., 2
(2), 91
–106
(2005). https://doi.org/10.1016/S1572-1000(05)00060-8 Google Scholar
L.-H. Wang, S. L. Jacques, and
L. Q. Zheng,
“MCML – Monte Carlo modeling of photon transport in multi-layered tissues,”
Comput. Methods Programs Biomed., 47
(2), 131
–146
(1995). https://doi.org/10.1016/0169-2607(95)01640-F Google Scholar
A. N. Yaroslavsky, P. C. Schulze, I. V. Yaroslavsky, R. Schober, F. Ulrich, and
H.-J. Schwarzmaier,
“Optical properties of selected native and coagulated human brain tissues in vitro in the visible and near infrared spectral range,”
Phys. Med. Biol., 47
(12), 2059
–2073
(2002). https://doi.org/10.1088/0031-9155/47/12/305 Google Scholar
J.-P. Ritz, A. Roggan, C. Isbert, G. Muller, H. J. Buhr, and
C.-T. Germer,
“Optical properties of native and coagulated porcine liver tissue between 400 and 2400 nm,”
Lasers Surg. Med., 29
(3), 205
–212
(2001). https://doi.org/10.1002/lsm.1134 Google Scholar
R. van Hillegersberg, J. W. Pickering, M. Aalders, and
J. F. Beek,
“Optical properties of rat liver and tumor at 633 nm and 1064 nm: photofrin enhances scattering,”
Lasers Surg. Med., 13
(1), 31
–39
(1993). https://doi.org/10.1002/lsm.1900130108 Google Scholar
A. M. K. Nilsson, R. Berg, and
S. Andersson-Engels,
“Measurements of the optical properties of tissue in conjunction with photodynamic therapy,”
Appl. Opt., 34
(21), 4609
–4619
(1995). https://doi.org/10.1364/AO.34.004609 Google Scholar
H.-J. Wei, D. Xing, J.-J. Lu, H.-M. Gu, G.-Y. Wu, and
Y. Jin,
“Determination of optical properties of normal and adenomatous human colon tissues in vitro using integrating sphere techniques,”
World J. Gastroenterol., 11
(16), 2413
–2419
(2005). Google Scholar
T. C. Zhu, A. Dimofte, J. C. Finlay, D. Stripp, T. Busch, J. Miles, R. Whittington, S. B. Malkowicz, Z. Tochner, E. Glatstein, and
S. M. Hahn,
“Determination of the distribution of light, optical properties, drug concentration, and tissue oxygenation in-vivo in human prostate during motexafin lutetium-mediated photodynamic therapy,”
J. Photochem. Photobiol., B, 79
(3), 231
–241
(2005). https://doi.org/10.1016/j.jphotobiol.2004.09.013 Google Scholar
J. W. Pickering, S. A. Prahl, N. van Wieringen, J. F. Beek, H. J. C. M. Sterenborg, and
M. J. C. van Gemert,
“Double-integrating-sphere system for measuring the optical properties of tissue,”
Appl. Opt., 32
(4), 399
–410
(1993). https://doi.org/10.1364/AO.32.000399 Google Scholar
G. de Vries, J. F. Beek, G. W. Lucassen, and
M. J. C. van Gemert,
“The effect of light losses in double integrating spheres on optical properties estimation,”
IEEE J. Sel. Top. Quantum Electron., 5 944
–947
(1999). https://doi.org/10.1109/2944.796315 Google Scholar
A. Roggan, M. Friebel, K. Dörschel, A. Hahn, and
G. Müller,
“Optical properties of circulating human blood in the wavelength range 400–2500 nm,”
J. Biomed. Opt., 4
(1), 36
–46
(1999). https://doi.org/10.1117/1.429919 Google Scholar
T. L. Troy and
S. N. Thennadil,
“Optical properties of human skin in the near infrared wavelength range of 1000 to 2200 nm,”
J. Biomed. Opt., 6
(2), 167
–176
(2001). https://doi.org/10.1117/1.1344191 Google Scholar
H.-J. Wei, D. Xing, G.-Y. Wu, H.-M. Gu, J.-J. Lu, Y. Jin, and
X.-Y. Li,
“Differences in optical properties between healthy and pathological human colon tissues using a Ti:sapphire laser: an in vitro study using the Monte Carlo inversion technique,”
J. Biomed. Opt., 10
(4), 044022
(2005). https://doi.org/10.1117/1.1990125 Google Scholar
M. Meinke, G. Müller, J. Helfmann, and
M. Friebel,
“Optical properties of platelets and blood plasma and their influence on the optical behavior of whole blood in the visible to near infrared wavelength range,”
J. Biomed. Opt., 12
(1), 014024
(2007). https://doi.org/10.1117/1.2435177 Google Scholar
M. Friebel, A. Roggan, G. Müller, and
M. Meinke,
“Determination of optical properties of human blood in the spectral range 250 to 1100 nm using Monte Carlo simulations with hematocrit-dependent effective scattering phase functions,”
J. Biomed. Opt., 11
(3), 034021
(2006). https://doi.org/10.1117/1.2203659 Google Scholar
E. Salomatina, B. Jiang, J. Novak, and
A. N. Yaroslavsky,
“Optical properties of normal and cancerous human skin in the visible and near-infrared spectral range,”
J. Biomed. Opt., 11
(6), 064026
(2006). https://doi.org/10.1117/1.2398928 Google Scholar
V. V. Tuchin,
“Optical properties of tissues with strong (multiple) scattering,”
Tissue Optics, 3
–17 SPIE Press, Bellingham, WA
(2007). Google Scholar
L.-H. V. Wang and
H. Wu,
“Scattering and its biological origins,”
Biomedical Optics: Principles and Imaging, 1
–16 Wiley, New York
(2007). Google Scholar
F. P. Bolin, L. E. Preuss, R. C. Taylor, and
R. J. Ference,
“Refractive index of some mammalian tissues using a fiber optic cladding method,”
Appl. Opt., 28
(12), 2297
–2303
(1989). https://doi.org/10.1364/AO.28.002297 Google Scholar
Oregon Medical Laser Center at Providence St. Vincent Medical Center: http://omlc.ogi.edu/spectra/hemoglobin/index.html Google Scholar
J. S. Nelson, L.-H. Liaw, A. Orenstein, W. G. Roberts, and
M. W. Berns,
“Mechanism of tumor destruction following photodynamic therapy with hematoporphyrin derivative, chlorin, and phthalocyanine,”
J. Natl. Cancer Inst., 80
(20), 1599
–1605
(1988). https://doi.org/10.1093/jnci/80.20.1599 Google Scholar
H. Joshima, M. Kashima, and
O. Matsuoka,
“Diminished osmotic fragility of mouse erythrocytes following intravenous injection of polymeric plutonium,”
J. Radiat. Res. (Tokyo), 25
(4), 290
–295
(1984). https://doi.org/10.1269/jrr.25.290 Google Scholar
X. Xu, R. K. Wang, J. B. Elder, and
V. V. Tuchin,
“Effect of dextran-induced changes in refractive index and aggregation of optical properties of whole blood,”
Phys. Med. Biol., 48 1205
–1221
(2003). https://doi.org/10.1088/0031-9155/48/9/309 Google Scholar
K. F. M. Fan, C. Hopper, P. M. Speight, G. A. Buonaccorsi, and
S. G. Bown,
“Photodynamic therapy using mTHPC for malignant disease in the oral cavity,”
Int. J. Cancer, 73
(1), 25
–32
(1997). https://doi.org/10.1002/(SICI)1097-0215(19970926)73:1<25::AID-IJC5>3.0.CO;2-3 Google Scholar
I. S. Saidi, S. L. Jacques, and
F. K. Tittel,
“Mie and Rayleigh modeling of visible-light scattering in neonatal skin,”
Appl. Opt., 34
(31), 7410
–7418
(1995). https://doi.org/10.1364/AO.34.007410 Google Scholar
R. Splinter and
B. A. Hooper,
“Light-tissue interaction variables,”
An Introduction to Biomedical Optics, 121
–154 Taylor & Francis, London
(2007). Google Scholar
P. R. Bargo, S. A. Prahl, T. T. Goodell, R. A. Sleven, G. Koval, G. Blair, and
S. L. Jacques,
“In vivo determination of optical properties of normal and tumor tissue with white light reflectance and an empirical light transport model during endoscopy,”
J. Biomed. Opt., 10
(3), 034018
(2005). https://doi.org/10.1117/1.1921907 Google Scholar
J. Swartling, J. Axelsson, G. Ahlgren, K. M. Kalkner, S. Nilsson, S. Svanberg, K. Svanberg, and
S. Andersson-Engels,
“System for interstitial photodynamic therapy with online dosimetry: first clinical experience of prostate cancer,”
J. Biomed. Opt., 15
(5), 058003
(2010). https://doi.org/10.1117/1.3495720 Google Scholar
M. S. Thompson, A. Johansson, T. Johansson, S. Andersson-Engels, S. Svanberg, N. Bendsoe, and
K. Svanberg,
“Clinical system for interstitial photodynamic therapy with combined on-line dosimetry measurements,”
Appl. Opt., 44
(19), 4023
–4031
(2005). https://doi.org/10.1364/AO.44.004023 Google Scholar
C. Fritsch, G. Goerz, and
T. Ruzicka,
“Photodynamic therapy in dermatology,”
Arch. Dermatol., 134 207
–214
(1998). https://doi.org/10.1001/archderm.134.2.207 Google Scholar
|