|
|
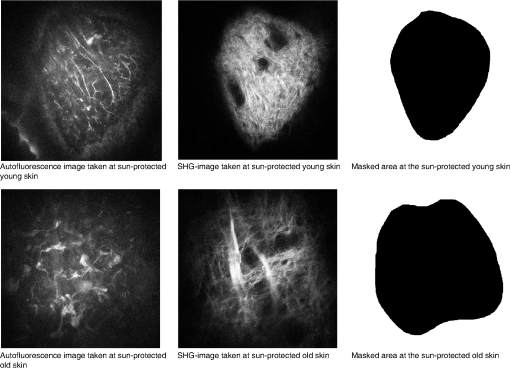
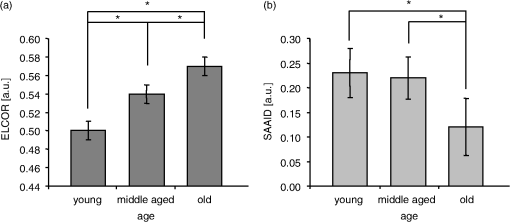
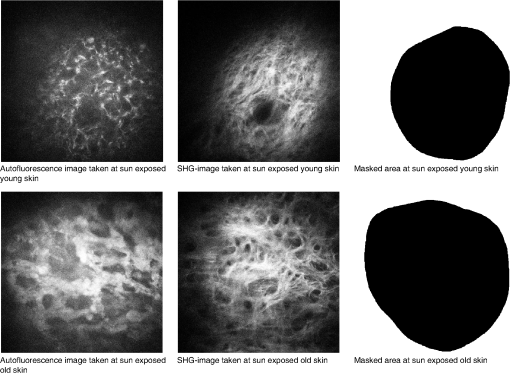
1.IntroductionHuman skin aging is a multifaceted phenomenon caused by intrinsic and extrinsic factors. While all human organs are subject to intrinsic aging, the process of extrinsic aging—mainly photoaging—is particularly prominent in human skin. Photoaging is superimposed on the inevitable intrinsic processes and is, to a large extent, due to environmental factors such as ultraviolet (UV) irradiation. Both types of aging induce profound changes in cutaneous morphology and structure. The physiology of the epidermis and dermis is altered, subsequently leading to increased fragility of the skin, laxity, and dry skin.1 Apart from collagen—the major component of the extracellular matrix (ECM)—the connective tissue contains an array of other components such as elastin, proteoglycans, fibronectin, and ECM proteins. In combination, these proteins are responsible for the dermal biomechanical properties. Whereas young skin is characterized by an intact, well-organized, and densely woven collagen network, this collagen is fragmented in the course of the aging process. At the same time, the synthesis of new collagen is down-regulated. Together these processes result in disorganized collagen fibers that accumulate within the ECM, impairing the structural integrity of the dermis.2–5 While elastin is a minor ECM component with regard to its weight percentage, it provides the crucial basis for cutaneous elasticity. In photoaged skin, however, normal elastic fibers are degraded.6 Elastotic material is deposited within the dermis forming amorphous structures and replacing the normal ECM structure and thus weakening skin resilience. In the past, dermal structures were mainly studied ex vivo using histological or ultrastructural methods. A drawback of these invasive approaches is the fact that skin biopsies must be taken to allow for ex vivo analyses. In the course of sample isolation (i.e., excision of skin biopsies), the mechanical forces built up by the collagen and elastin network are subject to change, which by itself impacts the overall dermal tissue structure, thus inevitably obscuring the actual ECM status and its structural organization. Noninvasive microscopic in vivo procedures (e.g., optical coherence tomography, Raman microspectrometry, in-vivo-confocal laser scanning microscopy) may be used to circumvent these issues for visualizing the human dermis in situ. However, these methods lack high resolution and/or functional imaging, which impairs the interpretation of results. To overcome these issues, we applied a multiphoton laser scanning microscope (MPLSM) for high-resolution three-dimensional in vivo imaging. This technique provides fast information under physiological conditions and is ideal to investigate age-associated dermal skin alterations quantitatively in vivo. It allows for the noninvasive evaluation of (extra)cellular structures by taking “optical” instead of a real skin punch biopsies without depending on contrasting agents. Here, dermal collagen fibers are visualized based on their ordered, noncentrosymmetric molecular structure giving rise to the collagen-specific second harmonic generation (SHG) signal. Elastin, on the other hand, emits autofluorescence (AF) signals that can be used for evaluation of elastic fibers or elastotic material. The MPLSM technology has already been used for a number of dermatological applications,7,8 for example, the investigation of collagen dissociation induced by chemicals,9 thermal denaturation of collagen,10 and effects of sunbed-induced skin aging.11 The aim of our study was to develop a parameter for the quantitative determination of dermal skin aging. We introduce the elastin-to-collagen ratio (ELCOR) as a new means to quantify accurately age-associated alterations in the ECM. 2.Materials and Methods2.1.Multiphoton Laser-Scanning MicroscopyFor noninvasive in vivo measurements avoiding the use of contrast agents, we developed, in collaboration with Jenlab GmbH (Jena, Germany), a CE marked multiphoton laser scanning microscope, called DermaInspect. This device contains a femtosecond laser, which provides a variable wavelength range (710 to 920 nm), a pulse repetition rate of 80 MHz, and a pulse width at the sample layer of about 150 fs. The DermInspect is equipped with a flexible mirror arm that allows optimal positioning over desired skin areas. To image the dermal fiber network in vivo, collagen-specific SHG signals were measured utilizing an irradiation wavelength of 820 nm and SHG was recorded using a specific band-pass filter (; AQ 410/20m-2P, Chroma Technology Corp., Bellows Falls, VT). Autofluorescence was determined using an excitation wavelength of 750 nm and emission was detected utilizing a band-pass filter (HQ 548/305m-2P, Schott AG, Mainz, Germany). For imaging parallel to the skin surface, the focus of the laser beam was scanned in vivo within the papillary dermis at depths of 30 and 45 µm beneath the basal membrane. Each scan was wide, and the image resolution was set at . 2.2.In Vivo StudiesAfter approval by an ethics committee, volunteers (ages 18 to 90 years) with skin types II and III were included in different in vivo studies. All donors provided written, informed consent. During the last 30 days prior to measurements, volunteers were required to desist from intensive sun exposure as well as visits to solariums. Also, the use of any medication two months prior to measurements was prohibited. Measurements were performed by trained and experienced personnel after acclimatization of volunteers for at least 30 min under standard atmospheric conditions ( and relative humidity). 2.3.Imaging of Intrinsic Aging In VivoTo study intrinsic aging in vivo using the MPLSM, SHG and AF signals of test areas located on the sun-protected volar side of one forearm of 45 healthy female subjects (15 young volunteers of ages 18 to 25; 15 middle-age volunteers of ages 35 to 45; and 15 older volunteers of ages years) were acquired. For measurements, the volunteers’ right forearms were placed on a special holder utilizing a specifically designed in vivo adapter that also allowed for correction of volunteers’ movements relative to the device. Areas of interest were imaged using two imaging modi at the same area. Each image was taken with 25 s acquisition time. We obtained AF images at 750 nm laser wavelength and SHG images at 820 nm laser wavelength. Images were taken at depths of 30 and 45 µm below the epidermal-dermal junction. All images were digitally stored for further quantitative analysis. 2.4.Imaging of Photoaging In VivoFor the characterization of photoaging effects, 12 elderly females ( years) were included in this study. Test areas were the sun-exposed temple area and sun-protected volar upper arm. Measurements were performed as previously described. To investigate the effect of different measuring depths on the elastin to collagen ratio (ELCOR), measurements were performed at depths of 30 and 45 µm and results were calculated independently for each depth. Acquisition time for each image was 13 s. Again, a mirror arm was used to guarantee optimal access to the test areas. 2.5.Quantification of Skin Aging by ELCORUsing the MPLSM data, the determination of the occupied area fractions of the AF signal of elastin and of the SHG signal of collagen were carried out as follows: After image acquisition, image preprocessing and image analysis were performed. First, nondermal structures were excluded. Second, deshading and denoising of images and also automatic threshold determination based on the gray-level histogram were carried out. Although the full image field that is occupied by either elastin or collagen fibers is used for analysis, in most cases, only a limited fraction of the entire image shows relevant fiber structures. The remaining parts may contain blood vessels or skin appendages. Because these structures interfere with the calculation of ELCOR, they are excluded by image-masking. The used masks are manually generated binary images. Next, the ELCOR parameter is determined as follows: Provided that the image most exclusively shows elastin fibers and the image primarily displays collagen fibers, the ratio of fibrous elastin to collagen tissue can be estimated from the corresponding occupied area fractions (OAFs) as follows: with being the area fraction of the (masked) image field that is occupied by elastin fibers in and analogously for being the area fraction of the (masked) image field that is occupied by collagen fibers in . Both OAF values can be calculated after binarization of the images and . Image binarization is conducted by automatic gray-level thresholding. Finally, is termed the elastin-to-collagen ratio (ELCOR).2.6.Quantification of Skin Aging by SAAIDFor both studies, the SHG to AF aging index of the dermis (SAAID) was calculated as described previously.12 In brief, index, calculated inside a masked area of . For validation of the ELCOR parameter, SAAID values were set in relation to previous studies that already demonstrated the age dependence of SAAID in vivo. 2.7.StatisticsA significance level of 0.05 (alpha) was chosen for statistical analysis, based on two-sided hypotheses. For other parameters, the following analyses were conducted: Imaging of intrinsic aging in vivo: Comparison among age groups via Mann-Whitney test. Imaging of photoaging in vivo: Comparison among test areas via Wilcoxon test. For analysis, Statistica and SAS software package for Windows V9.1.3 were used. 3.Results3.1.Determination of ELCOR in Intrinsic AgingTo investigate age-dependent effects in vivo, we compared the ELCOR parameter calculated from data collected at sun-protected young, middle-aged, and aged skin areas. Data were obtained at two different measurement depths and the average signal was used for calculation of the respective parameter. Figure 1 shows example images taken from sun-protected skin and their corresponding masks for young and aged volunteers. Figure 2(a) depicts the ELCOR parameter obtained from sun-protected volar skin (young: , ; middle age: , ; and older age: , ). With respect to volar skin, the ELCOR parameter significantly increased with age (young versus middle aged, ; middle aged versus old, ; young versus old, ). 3.2.Determination of ELCOR in PhotoagingBecause extrinsic factors predominantly determine human skin aging, we investigated the process of photoaging by MPLSM in elderly volunteers at different skin depths. The ELCOR parameter was determined and results from the sun-exposed temple area and the sun-protected upper arm were compared. Figure 3 shows example images taken from sun-exposed skin. As depicted in Fig. 4(a), at 30 µm below the basal membrane, the temple area yielded a value of compared to determined at 45 µm below the basal membrane. With respect to the sun-protected upper arm, the ELCOR parameter was calculated at 30 µm below the basal membrane compared to determined at 45 µm below the basal membrane. A significant difference between sun-exposed (temple skin) and sun-protected (upper arm skin) test areas in terms of ELCOR for elderly volunteers was detected at a depth of 30 µm (, ) and 45 µm (, ), respectively. Fig. 4ELCOR (a) and SAAID (b) values of test areas located on the chronically sun-exposed temple area and sun-protected upper arm. [Measurements were performed at depths of 30 and 45 µm below the basal membrane. Results are shown as (). Significant differences are marked with an asterisk (* for ).] 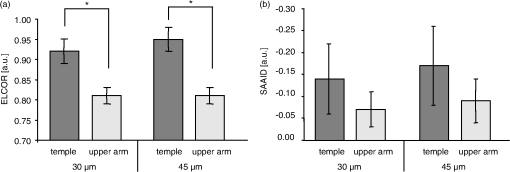 Compared to the sun-protected upper arm area, the ELCOR parameter calculated for the chronically sun-exposed temple area was significantly increased. 3.3.Comparison of ELCOR and SAAID ParametersUsing the data obtained in the in vivo study investigating intrinsic aging effects, the following SAAID parameters were calculated: ; ; ; and [Fig. 2(b)]. Because data were obtained at three different measurement depths, the average signal was used for calculation of the respective parameter. The SAAID parameter decreased with increasing age. However, not all investigated groups yielded significant differences (young versus middle aged, ; middle aged versus old, ; young versus old, ). As shown in Fig. 4(b), the respective SAAID parameter for the photoaging study are as follows: at 30 µm below the basal membrane, the temple area yielded a value of compared to determined at 45 µm below the basal membrane. The sun-protected upper arm showed an SAAID value of at 30 µm below the basal membrane compared to determined at 45 µm below the basal membrane. No significant differences between sun-protected and sun-exposed areas could be detected using the SAAID. 4.DiscussionSubstantial changes in the collagen network and the formation of elastotic material are characteristic features of photoaged skin. The assessment of these dermal changes is usually performed by subjective clinical evaluation in combination with histological and molecular analysis. Because this approach is invasive and cutaneous tissue architecture as well as mechanical properties are damaged during the excision of skin biopsies, the development of a noninvasive technique is crucial for diagnostic and research purposes. With the help of the high-resolution 3-D-MPLSM technology, it becomes possible to quantitatively investigate dermal skin alterations associated with photoaging and to determine extracellular characteristics of the ECM in vivo.11–13 Accordingly, the objective of this study was to devise a new parameter based on MPLSM technology that allows for the quantification of structural differences in chronically sun-exposed and intrinsically aged human skin in vivo. With respect to changes in the dermal ECM, the optical discrimination between collagen fibers and elastic fibers is achieved by measuring collagen-specific SHG signals and elastin-specific fluorescence signals, respectively. Several studies already successfully utilized MPLSM technology for dermatological research. In 2005, Lin et al.12 introduced the aging index of the dermis (SAAID) and suggested that SAAID can be used for the qualitative and quantitative characterization of alterations of dermal structures associated with photoaging. SAAID is defined as the difference between SHG and AF signals normalized to the sum of both signals: and currently represents the standard parameter used for determination of skin aging utilizing the in vivo MPLSM technology. Performing in vivo multiphoton laser measurements on the forearms of volunteers, Koehler et al.13,14 demonstrated that the SAAID parameter decreases with age and that the difference between sun-protected and sun-exposed skin areas increases during aging. A recent study also suggests that SHG and the SAAID index are useful indicators of facial skin aging in vivo.15 However, the use of SAAID is associated with certain restrictions. First, for determination of SAAID, only a small subregion of the entire dermis image is used for analysis. Furthermore, the subregion of interest is positioned subjectively in an ideally even illuminated image region. Second, it has to be noted that a comparison between different studies is delicate because SAAID can vary between positive or negative values. To overcome these disadvantages, we developed a more robust parameter, the elastin-to-collagen ratio, termed ELCOR. Based on the measurement of the elastin-specific AF signal and the collagen-specific SHG signal, the ELCOR parameter is defined as the ratio of the relative amount of elastin fibers to collagen fibers. Both the SAAID and the ELCOR parameter are based on similar input data (i.e., SHG and AF signal) and share several characteristics: First, with both the SAAID and the ELCOR parameter, a relative quantification of intrinsic skin aging and photoaging can be performed. Second, both methods are equally fast to carry out and calculate. Third, because ELCOR and SAAID are both mainly dependent on a pure AF elastin signal (w/o SHG) and a pure collagen SHG-signal (w/o AF of other components), optical filters in the measuring device have to assure pure signals. Apart from these common characteristics, the determination of the ELCOR parameter offers advantages. In contrast to SAAID, ELCOR is independent of total image intensity but based on image area comparisons instead. Also, most importantly, for the calculation of ELCOR, a large subregion of the entire image scan is employed for analysis. This is crucial because subjective image selection, as used with SAAID, can be ruled out completely. With respect to minimizing operator bias, this more objective approach appears to be quite favorable. Additionally, because ELCOR is calculated utilizing the quotient rather than the difference between SHG and AF signals, ELCOR offers the benefit of a more robust parameter because it is mostly independent of intensity scaling. In contrast, intensity scaling is relevant for the SAAID. In an earlier study using only the SHG signal, we already visualized the underlying structural changes in the collagen network of young and aged sun-exposed facial skin in vivo and determined collagen density changes in fibroblast-populated collagen gels.16 Employing the ELCOR parameter for the comparison of young, middle-aged, and aged sun-protected skin areas, our data now showed that the ELCOR parameter significantly increased with rising age of volunteers. Also, the ELCOR values of chronically sun-exposed areas were significantly higher than the ELCOR values determined at sun-protected skin areas of older volunteers. For the purpose of data validation and comparison, we determined for all ELCOR values calculated in this study, the corresponding SAAID values of young, middle-aged, and aged sun-protected skin areas and also of sun-protected and chronically sun-exposed areas of older skin. Taken together, these results demonstrate the validity of our experimental approach because decreasing SAAID values with age as well as lower SAAID values at sun-exposed compared to sun-protected skin areas are in line with the literature.11 However, in contrast to SAAID, ELCOR yielded significant results for all investigated groups and skin areas. As previously discussed, these significant differences are not due to the MPLSM measurement, but rather a benefit of improved image-analysis tools demonstrating the robustness and insusceptibility of the new parameter. Our data show that ELCOR increases with age and can be used as a tool to quantify intrinsic skin aging and photoaging. With respect to the investigation of photoaging, it has to be taken into account that ELCOR as well as SAAID were determined at different skin sides, the upper arm, and the temple area, which are characterized by a differing skin composition. Currently, we do not know which implications these different locations have on measurement parameters. We determined the ELCOR parameter at different depths below the basal membrane to investigate the dependence of ELCOR on measurement depth. A determination of parameters at measurement depths of both 30 and 45 µm below the basal membrane seems reasonable because this approach yielded statistically sound data. In conclusion, we introduced the ELCOR parameter based on the MPLSM technology as a means to study the cutaneous aging process in vivo. This novel parameter has proven useful to gain further insights into dermal skin aging and offers several advantages over the currently employed SAAID value. AcknowledgmentsFinancial support was obtained, in part, from the German Federal Ministry of Education and Research (BMBF, Grant no. 13N9282) and Beiersdorf AG. ReferencesL. H. Kligman,
“Photoaging, manifestations, prevention and treatment,”
Clin. Geriatr. Med., 5
(1), 235
–251
(1989). 0749-0690 Google Scholar
S. E. Fligielet al.,
“Collagen degradation in aged/photodamaged skin in vivo and after exposure to matrix metalloproteinase-1 in vitro,”
J. Invest. Dermatol., 120
(5), 842
–848
(2003). http://dx.doi.org/10.1046/j.1523-1747.2003.12148.x JIDEAE 0022-202X Google Scholar
A. OikarinenM. Kallioinen,
“A biochemical and immunohistochemical study of collagen in sun-exposed and protected skin,”
Photodermatol., 6
(1), 24
–31
(1989). PPPHEW 0905-4383 Google Scholar
J. Varaniet al.,
“Decreased collagen production in chronologically aged skin: roles of age-dependent alteration in fibroblast function and defective mechanical stimulation,”
Am. J. Pathol., 168
(6), 1861
–1868
(2006). http://dx.doi.org/10.2353/ajpath.2006.051302 AJPAA4 0002-9440 Google Scholar
J. Uitto,
“The role of elastin and collagen in cutaneous aging: intrinsic aging versus photoexposure,”
J. Drugs Dermatol., 7
(2 Suppl), s12
–16
(2008). JDDOBA 1545-9616 Google Scholar
V. L. Chenet al.,
“Immunochemistry of elastotic material in sun-damaged skin,”
J. Invest. Dermatol., 87 334
–337
(1986). http://dx.doi.org/10.1111/1523-1747.ep12524421 JIDEAE 0022-202X Google Scholar
K. König,
“Clinical multiphoton tomography,”
J. Biophotonics, 1
(1), 13
–23
(2008). http://dx.doi.org/10.1002/(ISSN)1864-0648 JBOIBX 1864-063X Google Scholar
S. J. LinS. H. JeeC. Y. Dong,
“Multiphoton microscopy: a new paradigm in dermatological imaging,”
Eur. J. Dermatol., 17
(5), 361
–366
(2007). EJDEE4 1167-1122 Google Scholar
T. Yehet al.,
“Reversible dissociation of collagen in tissues,”
J. Invest. Dermatol., 121
(6), 1332
–1335
(2003). http://dx.doi.org/10.1046/j.1523-1747.2003.12634.x JIDEAE 0022-202X Google Scholar
Y. Sunet al.,
“Investigating mechanisms of collagen thermal denaturation by high resolution second-harmonic generation imaging,”
Biophys. J., 91
(7), 2620
–2625
(2006). http://dx.doi.org/10.1529/biophysj.106.085902 BIOJAU 0006-3495 Google Scholar
M. J. Koehleret al.,
“Intrinsic, solar and sunbed-induced skin aging measured in vivo by multiphoton laser tomography and biophysical methods,”
Skin Res. Technol., 15
(3), 357
–363
(2009). http://dx.doi.org/10.1111/srt.2009.15.issue-3 0909-752X Google Scholar
S. J. Linet al.,
“Evaluating cutaneous photoaging by use of multiphoton fluorescence and second-harmonic generation microscopy,”
Opt. Lett., 30
(17), 2275
–2277
(2005). http://dx.doi.org/10.1364/OL.30.002275 OPLEDP 0146-9592 Google Scholar
M. J. Koehleret al.,
“In vivo assessment of human skin aging by multiphoton laser scanning tomography,”
Opt. Lett., 31
(19), 2879
–2881
(2006). http://dx.doi.org/10.1364/OL.31.002879 OPLEDP 0146-9592 Google Scholar
M. J. Koehleret al.,
“Morphological skin ageing criteria by multiphoton laser scanning tomography: non-invasive in vivo scoring of the dermal fibre network,”
Exp. Dermatol., 17
(6), 519
–523
(2008). http://dx.doi.org/10.1111/j.1600-0625.2007.00669.x EXDEEY 0906-6705 Google Scholar
K. Sugataet al.,
“Evaluation of photoaging in facial skin by multiphoton laser scanning microscopy,”
Skin Res. Technol., 17
(1), 1
–3
(2011). http://dx.doi.org/10.1111/srt.2011.17.issue-1 0909-752X Google Scholar
F. Fischeret al.,
“Folic acid and creatine improve the firmness of human skin in vivo,”
J. Cosmet. Dermatol., 10
(1), 15
–23
(2011). http://dx.doi.org/10.1111/jcd.2011.10.issue-1 JCDSEI 2161-4105 Google Scholar
|