|
|
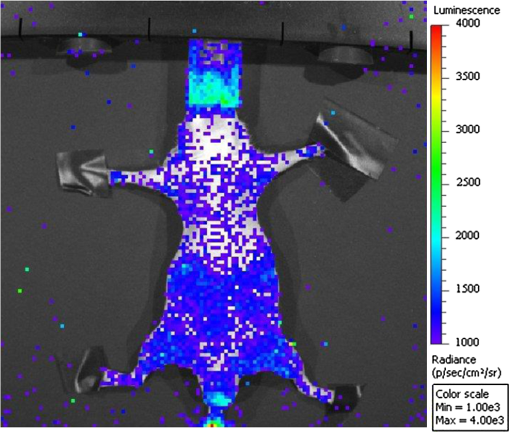
1.IntroductionRadioisotope luminescence imaging (RLI) is a novel optical imaging technique based on the detection of visible photons generated by processes related to nuclear decays.1 Within the RLI field, Cerenkov luminescence imaging (CLI) is a very fast-growing technique2–9 based on the detection of light generated when charged particles travel in a dielectric with a velocity greater than the speed of light in the medium itself. The energy threshold for Cerenkov radiation (CR) emission is dependent on the medium. For example, the threshold for a beta particle travelling in water is around 263 keV. CLI allows the detection of CR generated by both beta plus and beta minus emitters with an endpoint energy greater than the threshold. Preclinical visualization of the thyroid gland using CR was investigated in mice by Jeong in 2011 (Ref. 10), and recently our group obtained the first Cerenkov image of a human thyroid of a patient treated with for hyperthyroidism.11 As mentioned before, beta emitters with endpoint energy greater than the Cerenkov threshold are visible with CLI. However, despite the smaller light output, alpha and gamma emitters are also visible via RLI. The imaging of alpha emitters was developed recently using (Ref. 12) and (Ref. 13) and we demonstrated that the faint emission from biological tissues using alpha emitters is detectable with a conventional optical imager equipped with a charge-coupled device (CCD) camera. In a preliminary work,14 we investigated the in vivo imaging of -methylene-diphosphonate (-MDP) by using a small animal optical imaging system and covering the animal with a slab of bismuth germanate scintillating material. In a subsequent work,15 particular attention was focused on investigating the luminescence induced by without any scintillating materials. More precisely, we measured the time decay of the optical signal in a vial containing and we performed in vivo imaging using -sestamibi and -MPD. In conventional nuclear medicine, () is commonly used as a substitute for for the imaging of thyroid.16 More precisely, the uptake of -pertechnetate into the thyroid tissue is mediated by the sodium-iodide symporter (NIS), a transmembrane glycoprotein that actively mediates iodide (and other anions like ) transport into the thyroid follicular cells and several extrathyroidal tissues. Pertechnetate is thus used as an alternative medium for imaging of NIS-dependent functions, like transport of substrate into the thyroid gland and secretory function of the salivary glands and gastric mucosa.11 The biodistribution of pertechnetate has been well characterized in the past showing that the principal NIS-bearing tissues are the thyroid, salivary glands, and the stomach.17,18 Like and , -pertechnetate has a long and successful history of use in the diagnosis of thyroid cancer; moreover NIS expression has been found in more than 80% of human mammary cancers, and, thus, NIS has emerged as a potential target for radiotherapy of nonthyroid malignancies that express the endogenous or transfected symporter.17 This work can be considered a proof of principle; more precisely, the main goal of this paper is to show for the first time that using optical methods it is possible to image the parotid glands and the thyroid of a mouse injected with -pertechnetate. In our opinion this result can be useful considering the large availability and the moderate costs of preclinical optical imaging devices with respect to small animals single photon emission tomography (SPECT) scanners. 2.Materials and Methods2.1.RLI AcquisitionRLI images were acquired by using the Spectrum animal imaging system (Perkin-Elmer, Hopkinton, USA). The instrument is equipped with a cooled () back-thinned, back-illuminated CCD camera. The CCD has an active array of with a dimension of 13 microns. RLI data in vivo and ex vivo were obtained by acquiring images with the following parameters: exposure , , binning , without emission filter. The dynamic RLI data were acquired every 5 min. Light radiance measurements were done on regions of interest manually drawn over the animal’s neck; the luminescence signals are expressed as photons per seconds per squared centimeter per steradian (). Images were acquired and analyzed with Living Image 4.2 (Perkin-Elmer) and were corrected for the dark measurements. 2.2.Animal HandlingA total of six nude mice of were injected in the tail vein with about of 0.9% NaCl of -pertechnetate. Nude mice were used in order to allow the detection of a small number of optical photons. Mice were placed in a supine position 15 min before the imaging session in order to reduce the persistent luminescence that is responsible for the background noise in the case of luminescence images.19 During images acquisition, the mice were kept under gaseous anesthesia (2% of isoflurane and of oxygen). In order to optimize and image the thyroid uptake,18 three animals were sacrificed 35 min after injection and the salivary glands were removed. Three animals were imaged continuously for 70 min, mainly to investigate in vivo the salivary glands’ uptake.18 The specificity of RLI thyroid and salivary glands imaging with -pertechnetate was investigated using a control mouse injected in the tail vein with of -MDP. This tracer is known to be not thyroid specific, binding mainly to the bony structures of the animal. All the animal handling was approved by the Institutional Ethical Committee according to the regulations of the Italian Ministry of Health and the European Communities Council () directives. 3.ResultsIn this section, we present the results obtained from the in vivo and ex vivo experiments described in Sec. 2. Figure 1 shows an RLI image of two animals 35 min after injection of -pertechnetate. As one can see by looking at the image, both mice reveal light emission from anatomical regions corresponding to the salivary glands, thyroid, and stomach-intestine. Fig. 1RLI image of the -pertechnetate distribution in Nu/Nu mice placed in supine position. The zoomed regions corresponding to salivary-thyroid gland and along with the stomach-intestine are the most important sources of light emission. 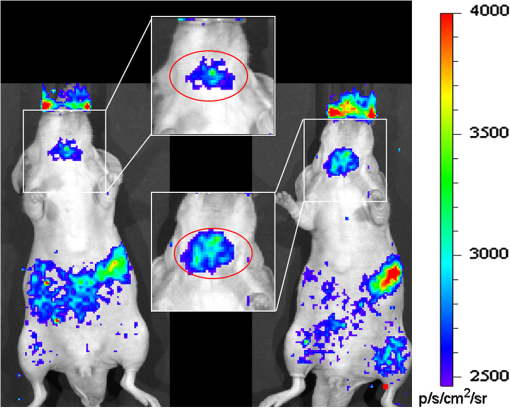 As shown by the time activity curve in Fig. 2, RLI dynamic imaging reveals a monotonic uptake of the radiopharmaceutical in the salivary glands-thyroid with respect to a background region. Fig. 2Average radiance () measured on ROIs corresponding to the salivary glands-thyroid and a background region. Dynamic data were acquired for 70 min after -pertechnetate injection. The measured radiance was obtained from a single mouse and the error bars correspond to the standard deviation of the radiance within the ROI.  In this case, the signal to background ratio of the salivary glands region measured after 70 min from the tracer injection was found to be equal to 1.85. These results prove that the -pertechnetate accumulated in the salivary glands anatomical district is visible with RLI and detectable over the background emission. Thirty-five minutes after -pertechnetate injection, three animals were sacrificed and the skin removed in order to visualize the thyroid and salivary glands. More precisely, with the aim of separating the signal contribution of the salivary glands with respect to the signal from the thyroid, the salivary glands were extracted from the body and imaged separately. Luminescence images were acquired as reported in Fig. 3(a). The image shows the light signal coming from the salivary glands complex in situ. The most relevant signal comes from the upper part of the glands in the rostro-caudal direction. Fig. 3The panel (a) shows an RLI image of the -pertechnetate distribution in the salivary glands in situ; the emission of the extracted salivary glands is presented in panel (b). Panel (d) shows the emission from the thyroid gland in situ with respect to the anatomical image (photograph) presented in panel (c). 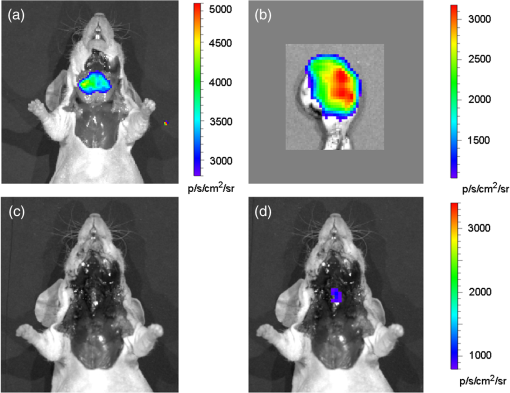 Figure 3(b) shows the light emission from the salivary glands alone, and in order to visualize the contribution of the very small murine thyroid gland, the mice were imaged again after the extraction of the salivary glands. Figure 3(d) shows the emission coming from the thyroid gland in situ; the localization of the light source is well in accordance with the corresponding anatomical position as shown in Fig. 3(c). The total flux escaping from the thyroid gland is about one order of magnitude less than the flux escaping from the salivary glands. Figure 4 shows an RLI of a control mouse injected in the tail vein with of -MDP. As expected, no specific salivary-thyroid binding of the tracer can be found. 4.Discussions and ConclusionsIn this work, we showed the first evidence of detectability of -pertechnetate using an optical imaging technique in living mice. The luminescence signal in the salivary and the thyroid glands were also measured ex vivo. The RLI dynamic data shown in Sec. 3 are in accordance with the results obtained using conventional nuclear medicine imaging with a gamma camera.17,18 We found that the total flux escaping from the thyroid gland is one order of magnitude less than the flux escaping from the salivary glands. Moreover, the thyroid gland is located deeper inside the tissue when the animals are in a supine position, so it is possible to argue that the contribution of the signal escaping from the living animals is due mainly to the salivary glands uptake. We would like to underline here that with the term salivary glands we are referring to the submandibular-sublingual complex (SSC), which is composed of the submandibular and sublingual glands located in the ventral cervical region. The submandibular gland is almond-shaped and the sublingual gland lens-shaped, lying lateral to the rostral third of the submandibular gland. The two glands are separated by a thin sheet of connective tissue and the excretory ducts emerge rostrally from both glands.20 The submandibular gland is mainly composed of serous cells and the sublingual gland is mainly composed of mucous cells. The nonhomogeneity of light signal detected in the salivary glands could suggest different uptakes of -pertechnetate in the glands themselves and could reflect different functionalities of the two components of the SSC, but this hypothesis needs to be further investigated. Results obtained using a control mouse injected with -MDP showed, as predicted, no specific salivary-thyroid binding with respect to -pertechnetate. In conclusion, the luminescence images presented in this work reveal that -pertechnetate uptake in NIS-expressing cells were well visualized using a commercial optical imager instrument, and, thus, RLI with -pertechnetate has potential applications for salivary glands and thyroid gland research in small animals. This result suggests that -pertechnetate could be used in the future to image NIS-bearing cancer cells that can be found in 80% of human mammary cancers. AcknowledgmentsThe authors would like to acknowledge the Cariverona Foundation for financial support. ReferencesA. E. Spinelliet al.,
“Optical imaging using radioisotopes: a novel multimodal approach to molecular imaging,”
Q. J. Nucl. Med. Mol. Imag., 56
(3), 279
–289
(2012). Google Scholar
R. Robertsonet al.,
“Optical imaging of Cerenkov light generation from positron-emitting radiotracers,”
Phys. Med. Biol., 54
(16), N355
–N365
(2009). http://dx.doi.org/10.1088/0031-9155/54/16/N01 PHMBA7 0031-9155 Google Scholar
A. E. Spinelliet al.,
“Cerenkov radiation allows in vivo optical imaging of positron emitting radiotracers,”
Phys. Med. Biol., 55
(2), 483
–495
(2010). http://dx.doi.org/10.1088/0031-9155/55/2/010 PHMBA7 0031-9155 Google Scholar
F. Boschiet al.,
“In vivo (18)F-FDG tumour uptake measurements in small animals using Cerenkov radiation,”
Eur. J. Nucl. Med., 38
(1), 120
–127
(2011). http://dx.doi.org/10.1007/s00259-010-1630-y EJNMD9 0340-6997 Google Scholar
A. E. Spinelliet al.,
“Cerenkov radiation imaging of beta emitters: in vitro and in vivo results,”
Nucl. Instrum. Meth. A, 648
(Suppl 1), S310
–S312
(2011). http://dx.doi.org/10.1016/j.nima.2010.11.038 NIMAER 0168-9002 Google Scholar
A. E. Spinelliet al.,
“Multispectral Cerenkov luminescence tomography for small animal optical imaging,”
Opt. Express, 19
(13), 12605
–12618
(2011). http://dx.doi.org/10.1364/OE.19.012605 OPEXFF 1094-4087 Google Scholar
A. E. SpinelliF. Boschi,
“Unsupervised analysis of small animal dynamic Cerenkov luminescence imaging,”
J. Biomed. Opt., 16
(12), 120507
(2011). http://dx.doi.org/10.1117/1.3663442 JBOPFO 1083-3668 Google Scholar
F. Boschiet al.,
“Quantum dots excitation using pure beta minus radioisotopes emitting Cerenkov radiation,”
RSC Advances, 2
(29), 11049
–11052
(2012). http://dx.doi.org/10.1039/c2ra22101b RSCACL 2046-2069 Google Scholar
A. E. SpinelliF. Boschi,
“Optimizing in vivo small animal Cerenkov luminescence imaging,”
J. Biomed. Opt., 17
(4), 040506
(2012). http://dx.doi.org/10.1117/1.JBO.17.4.040506 JBOPFO 1083-3668 Google Scholar
S. Y. Jeonget al.,
“Combined Cerenkov luminescence and nuclear imaging of radioiodine in the thyroid gland and thyroid cancer cells expressing sodium iodide symporter: initial feasibility study,”
Endocr. J., 58
(7), 575
–583
(2011). http://dx.doi.org/10.1507/endocrj.K11E-051 EDJUE6 0969-711X Google Scholar
A. E. Spinelliet al.,
“First human Cerenkography,”
J. Biomed. Opt., 18
(2), 020502
(2013). http://dx.doi.org/10.1117/1.JBO.18.2.020502 JBOPFO 1083-3668 Google Scholar
A. Ruggieroet al.,
“Cerenkov luminescence imaging of medical isotopes,”
J. Nucl. Med., 51
(7), 11231130
(2010). http://dx.doi.org/10.2967/jnumed.110.076521 JNMEAQ 0161-5505 Google Scholar
F. Boschiet al.,
“Optical imaging of alpha emitters: simulations, phantom, and in vivo results,”
J. Biomed. Opt., 16
(12), 126011
(2011). http://dx.doi.org/10.1117/1.3663441 JBOPFO 1083-3668 Google Scholar
F. Boschiet al.,
“Combined optical and single photon emission imaging: preliminary results,”
Phys. Med. Biol., 54
(23), L57
–L62
(2009). http://dx.doi.org/10.1088/0031-9155/54/23/L01 PHMBA7 0031-9155 Google Scholar
A. E. Spinelliet al.,
“Optical imaging of Tc-99m based tracers, in vitro and in vivo results,”
J. Biomed. Opt., 16
(11), 116023
(2011). http://dx.doi.org/10.1117/1.3653963 JBOPFO 1083-3668 Google Scholar
U. Y. Ryoet al.,
“Thyroid imaging agents: a comparison of I-123 and Tc-99m pertechnetate,”
Radiology, 148
(3), 819
–822
(1983). RADLAX 0033-8419 Google Scholar
L. S. Zuckieret al.,
“Kinetics of perrhenate uptake and comparative biodistribution of perrhenate, pertechnetate, and iodide by NaI symporter–expressing tissues in vivo,”
J. Nucl. Med., 45
(3), 500
–507
(2004). JNMEAQ 0161-5505 Google Scholar
P. R. Frankenet al.,
“Distribution and dynamics of -pertechnetate uptake in the thyroid and other organs assessed by single-photon emission computed tomography in living mice,”
Thyroid, 20
(5), 519
–526
(2010). http://dx.doi.org/10.1089/thy.2009.0213 THYRER 1050-7256 Google Scholar
F. Boschiet al.,
“Spontaneous luminescence background in living Nu/Nu mice,”
Adv. Mol. Imaging, 2
(2), 5
–11
(2012). http://dx.doi.org/10.4236/ami.2012.22002 Google Scholar
A. Sbarbatiet al.,
“Magnetic resonance imaging of the submandibular-sublingual complex,”
Acta Anatomica, 149
(1), 63
–69
(1994). http://dx.doi.org/10.1159/000147556 ACATA5 0001-5180 Google Scholar
|