|
|
|
A lumpectomy (also known as breast-conserving surgery) is a common surgical procedure for the removal of small and impalpable breast lesions,1,2 in which a breast lump is resected with a surrounding rim of normal tissue. This helps to preserve the general shape of the breast to a greater extent than a mastectomy, which requires partial or complete excision of the breast.1 Identifying the location of the breast lesion to be excised prior to the lumpectomy is necessary for its effective surgical removal. A hookwire or Kopans wire is a standard tool for the preoperative localization of the breast lesion.3–5 The localization is achieved by passing a 25-cm long thin steel wire through a needle into the breast tissue under mammographic or ultrasonic guidance. The V-shaped tip of the wire end is anchored at the lesion site by sliding the needle out of the breast. The surgeon identifies the location of the anchored tip in the lesion by viewing x-ray mammograms or ultrasound images of the tip of the wire and tries to excise the tissue surrounding the tip. This procedure is heavily empirical and often leads to additional surgeries due to positive margins found in a subsequent biopsy. Dayton et al.6 have shown that the conventional metal wire-guided lumpectomy could be improved by using a piece of optical fiber. In their study, they attached a large-core () bare fiber parallel to a standard Kopans wire using medical glue. Light from a He-Ne laser was coupled into the fiber, so that the tip of the optical fiber illuminated the breast tissue and produced a glow ball of red laser light around the lesion. The glow ball immediately showed and localized the position of the fiber tip, thus assisting surgeons in locating and resecting the breast lesion. The same group reported clinical application of the optical wire to female patients suffering from high-grade ductal carcinoma in situ and provided improved margin states for the resection of small lesions.7 Despite its promising results, it is necessary to raise a few issues regarding the use of optical fiber as the optical wire. The conventional silica glass fiber is not suitable for human applications because of its stiffness and nonbiocompatibility. The fiber may be broken within the breast with a small unexpected impact, which can induce tissue damage such as bleeding or inflammation. Moreover, in order to deliver the light, patients need to keep a few meters long optical fiber wound and taped on their skins during the preoperation period, which can cause physical and psychological discomforts. Parker et al.8 have recently shown that the biopolymer materials, such as a silk fibroin, can serve as an optical waveguide to transport the light. From their finding, we hypothesize that indicating the lesion location can be possible using a biocompatible and flexible optical wire. In this paper, we propose a safe and biocompatible method of light-guided localization in tissue using an optical wire, the widely used surgical suture. We chose a conventional surgical suture (PDS II, Ethicon, Somerville, New Jersey) as the biocompatible photonic material. PDS II (polydioxanone) is a synthetic monofilament absorbable suture generally used in all types of soft tissue approximation including ophthalmic surgery.9 We reasoned that the homogeneity of the polymeric suture would allow the propagation of light through the material of the suture even within the tissue. This prediction was confirmed by a simple experiment shown in Fig. 1(a). As can be seen, we prepared two freshly sliced chicken breast tissues [20-mm thick, (Ref. 10)] and a 60-mm long, thick PDS II suture. One end of the suture was cleaved with a razor to facilitate the laser launching. One third of the suture (20-mm length) was sandwiched between the two chicken breast slices to mimic the optical wire embedded in tissue. A 20-mW He-Ne red laser (632.8 nm) beam was focused on the cleaved end of the suture through a objective lens (5723-H-B, 0.4 NA, New Focus, Santa Clara, California). In Fig. 1(b), strong scattering of the red laser light is observed within the tissue and at the point where the suture enters the tissue. It was observable even under ambient room illumination. Because the suture has no cladding layer, which is definitely necessary for a waveguide to confine the beam within the core layer, a great portion of the light travelling along the suture in air leaks out at the suture–tissue interface. We note that the refractive index of the suture material is higher than most biomaterials, like tissues, in general. However, the portion of the light that has passed the suture–tissue interface could propagate along the suture without appreciable scattering and finally yield an intense fan-like glow ball of light within the tissue, as indicated with the dotted circle in Fig. 1(b). This result shows the ability of the suture to guide the visible (red) light within the tissue in order for surgeons to be able to see the surgical area with naked eyes. Fig. 1(a) Schematic diagram of the experimental arrangement for light-guided localization in a chicken breast tissue using the surgical suture. (b) A photograph (top view) of (a) under ambient room lighting. A fan-like glow ball of light at the tip of the suture is visible in the tissue (the dotted circle). 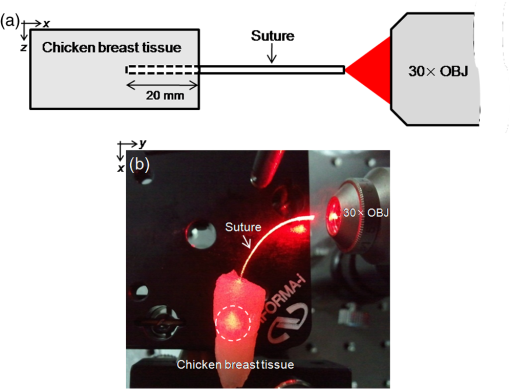 The coupling efficiency of the suture was measured to be about 10%. It is rather small for practical applications. However, considering that the commercial suture has been used as an optical waveguide without any modification, the coupling efficiency can be encouraging. Proper cleaving of the suture would improve the launching efficiency of the laser beam. The suture was cut with a razor in this experiment. Due to the flexibility and softness of the suture material, the cleaving method used for the brittle glass fiber can be inappropriate. As an optical waveguide, the suture should be investigated further. With regards to the real application of the suture to breast cancer patients, the length of the suture outside the breast needs to be shortened for two reasons: to reduce patient discomfort due to the suture and to avoid a strong bending loss caused by the highly flexible nature of the suture. In this scenario, it is difficult to directly launch the laser beam into the short suture near the breast. To resolve this difficulty, we adopted an optical coupling technique for launching the light to the suture through its side instead of through the end, which has been widely used to combine or split optical signals for fiber optic sensing or biomedical imaging.11,12 The contact coupling method is a good choice for simple and efficient optical coupling, where the optical power in the input fiber is partially coupled to the output fibers through physical contact.12,13 This suggests that light from a distant laser can be delivered to the output fiber (suture here) merely by touching or winding the input fiber from the side. In this study, we used a homemade double-cladding fiber (DCF) as an input fiber to feed light to the suture with the contact coupling method. The DCF is a specialty optical fiber having an outer cladding layer in addition to the conventional inner cladding layer. Owing to the lower refractive index of the outer cladding layer compared with the inner cladding layer, we can use the latter as a large area multimode waveguide.12,13 In our experiment, the outer cladding layer could be simply obtained by coating the conventional single-mode fiber with a resin of low-refractive index. The diameters of the core, the inner cladding layer, and the outer cladding layer were 10, 125, and , respectively.12 Figure 2(a) shows a schematic diagram of the contact coupling method using the DCF connected to a multimode fiber (MMF), with a core diameter of , through a fiber connector (FC). The other end of the MMF was patched to an output of a 2.5-mW fiber-pigtailed red laser. The outer cladding of the DCF was carefully peeled off along a 40-mm length so that the inner cladding could be exposed. Then, the DCF and the suture were twisted around each other about three turns at the outer cladding-peeled off region. A small amount of index matching oil (18061, Cargille Labs, Inc., Cedar Grove, New Jersey) was evenly applied to the twisted region to get a better contact. The refractive index of the oil was 1.458, slightly less than that of the inner cladding of 1.46. With this, the output He-Ne laser beam from the MMF could easily be launched into the inner cladding of the DCF and then substantially transferred to the suture. The optical coupling result is shown in Fig. 2(b), where the red light (arrow) is observed at the tip of the suture. We can see that its intensity is strong enough to be projected onto a paper sheet as in Fig. 2(c). The coupling efficiency from the MMF to the suture with the method of Fig. 2(a) was measured at about 0.9%. The low coupling efficiency is mainly due to the leakage of light at the contact region of the DCF coupler. Of course, adjusting the contact length and the number of the twisting turns may appreciably improve the coupling efficiency.12 More systematic and quantitative investigation on the optical properties of the suture is under consideration. However, the more important thing is making a cladding layer by coating the suture with a low-index biocompatible material, which is definitely necessary for the practical use of the suture as an optical waveguide. Fig. 2(a) Schematic diagram of light delivery using the double-cladding fiber (DCF) and the contact coupling method. S: suture, FC: fiber connector, and MMF: multimode fiber. (b) Photographic view of (a) taken in a dark room. The red light (arrow) at the tip of the suture is visible. (c) Light propagating through the suture and projected on a paper sheet. 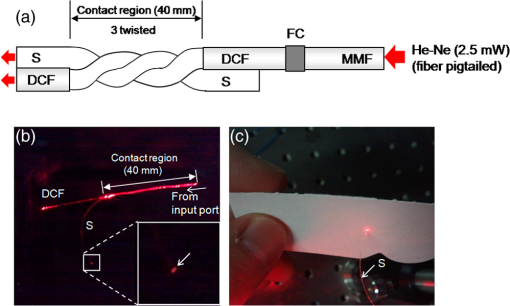 In order to test the light delivery property of the surgical suture and the light coupling property of the DCF coupler, we attempted the light-guided localization using another fresh chicken breast tissue, as shown in Fig. 3(a). The breast tissue was drilled using an injection needle, and the suture was carefully inserted 35 mm below the surface. Part of the suture outside the breast tissue was wound together with the DCF (10 turns), forming a 75-mm long contact region. The 20-mW laser beam was directly launched at the input end of the DCF using the same objective of Fig. 1. Figure 3(b) is the photograph of the experimental arrangement. In Fig. 3(c), we can clearly see a red glow ball (arrow) at the tip of the suture located within the tissue. The observation was made in a dark room. However, even under ambient illumination, as shown in Fig. 3(d), we could recognize the red glow ball with naked eyes. As was mentioned, the strong light at the suture–tissue interface means that we need to form a cladding layer to the suture with a low-index coating. Fig. 3(a) Schematic diagram of the experimental arrangement for light-guided localization in a chicken breast tissue. DCF: double-cladding fiber, S: suture, and OBJ: objective. (b) A photograph (top view) of (a). (c and d) Light-guided localization under dark and ambient illuminations, respectively. 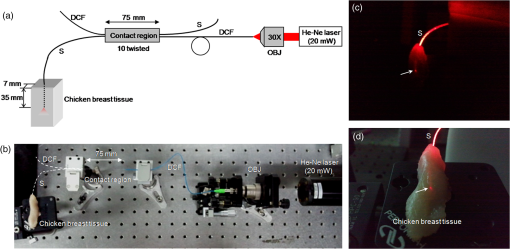 In conclusion, we have presented the effectiveness of biocompatible optical wire, such as a surgical suture, for light-guided localization in tissue. The surgical suture was used as the optical wire. The He-Ne laser beam was launched into the suture from its side with the help of DCF coupler. Just winding a suture around the DCF gave appreciable light coupling into the suture, and the coupled light could reach down to 35 mm within a chicken breast tissue. Even though preliminary, the experimental results suggest that our approach can be engineered into a practical optical wire that can indicate the location of a breast lesion with an easy, comfortable, and biocompatible way. Furthermore, laser treatment of the lesion through the optical wire, such as in photodynamic therapy, can be a functional advantage of this approach. AcknowledgmentsThis study was supported by a grant from the Korean Health Technology Research and Development Project of the Ministry of Health, Welfare and Family Affairs, Republic of Korea (No. A100490). ReferencesC. Kotwallet al.,
“Breast conservation surgery for breast cancer at a regional medical center,”
Am. J. Surg., 176
(6), 510
–514
(1998). http://dx.doi.org/10.1016/S0002-9610(98)00254-2 AJOOA7 0096-6347 Google Scholar
F. FitzalM. Gnant,
“Breast conservation: evolution of surgical strategies,”
Breast J., 12
(s2), S165
–S173
(2006). http://dx.doi.org/10.1111/tbj.2006.12.issue-s2 BRJOFK 1075-122X Google Scholar
M. J. Homer,
“Transection of the localization hooked wire during breast biopsy,”
Am. J. Roentgenol., 141
(5), 929
–930
(1983). http://dx.doi.org/10.2214/ajr.141.5.929 AJROAM 0092-5381 Google Scholar
W. B. Morrisonet al.,
“Preoperative CT-guided hookwire needle localization of musculoskeletal lesions,”
Am. J. Roentgenol., 176
(6), 1531
–1533
(2001). http://dx.doi.org/10.2214/ajr.176.6.1761531 AJROAM 0092-5381 Google Scholar
K. J. Brownet al.,
“Imaging-guided preoperative hookwire localization of nonpalpable extramammary lesions,”
Am. J. Roentgenol., 197
(3), W525
–W527
(2011). http://dx.doi.org/10.2214/AJR.10.6176 AJROAM 0092-5381 Google Scholar
A. Daytonet al.,
“Light-guided lumpectomy: device and case report,”
J. Biomed. Opt., 15
(6), 061706
(2010). http://dx.doi.org/10.1117/1.3499422 JBOPFO 1083-3668 Google Scholar
A. Daytonet al.,
“Light-guided lumpectomy: first clinical experience,”
J. Biophotonics, 4
(10), 752
–758
(2011). http://dx.doi.org/10.1002/jbio.v4.10 JBOIBX 1864-063X Google Scholar
S. T. Parkeret al.,
“Biocompatible silk printed optical waveguides,”
Adv. Mater., 21
(23), 2411
–2415
(2009). http://dx.doi.org/10.1002/adma.v21:23 ADVMEW 0935-9648 Google Scholar
S. H. Changet al.,
“Absorbable PDS-II suture and nonabsorbable polypropylene suture in aortic anastomoses in growing piglets,”
J. Formosan Med. Assoc., 97
(3), 165
–169
(1998). JFASEO 0929-6646 Google Scholar
G. Marquezet al.,
“Anisotropy in the absorption and scattering spectra of chicken breast tissue,”
Appl. Opt., 37
(4), 798
–804
(1998). http://dx.doi.org/10.1364/AO.37.000798 APOPAI 0003-6935 Google Scholar
B. H. Leeet al.,
“Specialty fiber coupler: fabrications and applications,”
J. Opt. Soc. Korea, 14
(4), 326
–332
(2010). http://dx.doi.org/10.3807/JOSK.2010.14.4.326 1226-4776 Google Scholar
S. Y. Ryuet al.,
“The development of double-clad fiber and double clad fiber coupler for fiber based biomedical imaging systems,”
J. Opt. Soc. Korea, 13
(3), 310
–315
(2009). http://dx.doi.org/10.3807/JOSK.2009.13.3.310 1226-4776 Google Scholar
S. Y. Ryuet al.,
“A fiber-based single-unit dual-mode optical imaging system: swept source optical coherence tomography and fluorescence spectroscopy,”
Opt. Commun., 285
(9), 2478
–2482
(2012). http://dx.doi.org/10.1016/j.optcom.2011.12.098 OPCOB8 0030-4018 Google Scholar
|

