|
|
|
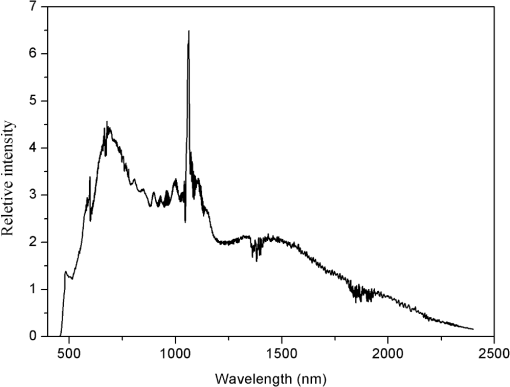
Supercontinuum (SC) is becoming a hot research topic across the world in recent years, owing to the rapid developments in diode pumping and fiber fabrication technologies.1 As the applications of SC sources are broadly extended, concerns should be raised regarding their safety for human health and particularly potential harmful risks for the eye. It is known that only milliwatts or microjoules orders of magnitude for a visible laser could induce irreversible damage to the retina.2 Nowadays, the output of commercial SC sources has reached above 10 W,3 and the spectrum is primarily composed of visible and near-infrared radiations, which are the most harmful wavelength bands for the retina. Furthermore, it may be very difficult to protect the eyes from the damage induced by SC sources, since no protective eyewear can provide an effective defense against the broadband SC under the condition of the vision function remaining normal. However, no experimental or theoretical study about the ocular damage induced by SC has ever been performed. Meanwhile, the current safety guidelines for neither the laser nor the incoherent light source covers this new kind of artificial light source.4,5 Therefore, it may be necessary to investigate the ocular damage effect induced by SC, which will provide some theoretical and experimental foundations for its safety standard. In this paper, experiments were conducted to determine the retinal damage threshold of chinchilla grey rabbits induced by a Vis-infrared (IR) SC source. To our knowledge, this is the first investigation about this new light source. The SC source (National University of Defense Technology) produced about 6-ns pulses at a repetition rate of 400 kHz with a maximum average power of 6.97 W, covered the wavelength range from 450 nm to 2400 nm, and was collimated at the wavelength of about 550 nm using a lens-based collimator. Figure 1 was the measured spectrum of the source at the maximum output. Some neutral density attenuators (Daheng Optics, Beijing, China) were used to adjust the incident power. The transmittances of these attenuators were nearly constant from wavelengths of 450 to 2400 nm, which kept the spectral distribution of the SC source unchanged. The exposure time and the spot size on the cornea were set to 0.1 s and 5 mm, respectively. Chinchilla grey rabbits of either sex weighing 2.0 to 2.6 kg were used for the experiments. The animals were procured and maintained in the Center for Laboratory Animal Medicine and Care, Beijing, China and used in accordance with the institutional guidelines of the Animal Care and Use Committee and the ARVO Resolution on the Use of Animals in Research. The rabbits were anesthetized with an intramuscular injection of a mixture of ketamine hydrochloride () and xylazine (). Full pupil dilation was performed with two drops of proparacaine hydrochloride 0.5%, phenylephrine hydrochloride 2.5%, and tropicamide 1% at a 5-min interval. A pilot study was conducted to generate damages from no visible burn to retinal contained hemorrhage. From the 24-h post-exposure readings, we estimated the approximate range of the retinal damage threshold. Based on the estimation, four levels of power ranged from 51.1 to 92.7 mW were chosen in the subsequent experiment to determine the threshold, and six rabbits (12 eyes) were involved. For each eye, two levels of dose (each dose with ten exposures) were delivered to the eye fundus. Following each exposure session, lesion/no lesion determinations were made for each exposure site by two experienced investigators. Meanwhile, the corneas and lens were also examined with a slit lamp to determine whether the anterior components of the eye were damaged by the infrared components of the SC source. Examinations were performed at 1, 24, and 48 h after exposure. The lesion/no lesion data were collected and analyzed using an SAS statistical package (version 6.12, SAS Institute, Inc., Cary, NC). Bliss probit analysis was performed to determine the thresholds, fiducial limits at the 95% confidence level and probit slopes (). To determine the mechanisms of irradiation effects of the SC on the retina, qualitative histopathologic studies for different damage levels were also performed. Some of the rabbits were euthanized at 24 h after exposure and the eyeballs were taken and fixed in Davidson solution for 24 h, then dehydrated with ethanol, embedded with paraffin, serially sectioned, and the sections stained with hematoxylin and eosin (H&E). It was shown that no corneal or lens damage could be found even for the highest power, but retinal damage was observed. This could be explained as follows. First, because of the transparency of the ocular media, the inherent focusing properties of the eye, and the absorption of the melanin, the retina is much more susceptible to damage by radiation in the region from 400 to 1400 nm (retinal hazard region) than other parts. Furthermore, the component of the SC source in the region 400 to 1400 nm accounts for about 71% of the total spectrum. Therefore, the retina is the most effected tissue in our experiment. Results of the retinal threshold were given in Table 1 for the 1- and 24-h readings together with their fiducial limits at the 95% confidence level. In addition, the probit slopes were shown in the last column for each observation time. The threshold at 24 h was lower than the value at 1 h, but after 24 h, the number of lesions remained constant and the threshold at 48 h was the same as the value at 24 h. In determining , the probit slope reflects the total experimental uncertainty. It was shown that the probit slopes were 1.19 and 1.29 in Table 1, which was a good indication of the overall uncertainty and quality of the experimental data.6 Table 1Summary of the data for retinal damage thresholds induced by SC source.a
For analyzing the hazard risks of SC, a theoretical method was also developed to calculate the effective exposure dosage. Owing to the similar characteristics between SC source and laser (high brightness, good direction), it is appropriate to use “radiant exposure” (expressed in ) as the exposure dosage. However, due to the dependence of the damage threshold on the retinal spot size, the retinal image size must be provided when comparing damage thresholds between SC and laser. On the other hand, SC sources have another unique characteristic, i.e., super broadband spectrum; thus, we should introduce the retinal hazard spectral weighting function,4 which characterizes the spectral efficiency to cause threshold retinal damage and has been used for evaluating the hazard risks of incoherent light sources. In this way, we could introduce the quantity “effective radiant exposure” to describe the exposure dosage of the SC source. The total power of an SC source can be expressed as where is the relative spectral intensity at the wavelength and represents the proportionality coefficient. By introducing the retinal hazard spectral weighting function , the effective power can be expressed as where and represent the lower and upper action bounds. For retinal thermal damage, is 380 nm, and is 1400 nm.4 Combined with the spot size at the cornea and the exposure time , the “effective radiant exposure” can be calculated byFor laser, is determined by where is the “radiant exposure” of the laser.Using above method and experimental parameters, the corresponding to the 24-h threshold was . When comparing retinal damage thresholds for different corneal spot sizes, the total intraocular energy (TIE) is believed more suitable than corneal radiant exposure.5 Thus, the threshold expressed in TIE was also calculated (2.4 mJ). In order to compare our result with other results or MPE values, the retinal spot size must be provided. According to the light micrographs and the fundus photographs of the lesion, the estimated spot size was about . Lund et al.7 reported the damage thresholds at different retinal spot sizes for 0.1 s duration exposures to 514-nm laser irradiation. At , the damage threshold was about 1.68 mJ, which was close to our value. For the laser with the wavelength between 400 and 700 nm, the MPE value expressed in TIE is 0.59 mJ with an exposure time of 0.1 s and retinal image size of .5 Similarly, for the incoherent light source, the MPE value is 0.77 mJ. It was shown that a sufficient margin existed between the damage threshold and the MPE value for both the laser or for the incoherent light source. Similarly, the “effective radiant exposure” for the cornea could also be calculated by introducing the corneal thermal hazard spectral weighting function.4 For the thermal damage of the cornea, is 780 nm and is the upper bound of the SC source. The for the cornea was when the incident power was 92.7 mW. For infrared bands larger than 1400 nm, the lowest MPE value of the laser is . For the incoherent light source, the MPE value is . It was shown that the for the largest incident power used in the experiment was far lower than the MPE value for either the laser or the incoherent light source. In other words, the cornea would not be damaged under our experimental conditions. The above theoretical analysis was consistent with the experimental result. Figure 2(a) showed the lesions induced by the SC source. Grossly, the damage induced by the SC source appeared as circular, well-demarcated, white, and opaque lesions. The retinal damage appearance induced by the SC source was similar to that of laser. This was because the SC source had similar characteristics to the laser, i.e., good direction and high brightness. Figure 2(b) showed the light micrograph of the lesion corresponding to the near-threshold damage (78.3 mW), where a slight alteration of the retinal pigment epithelium (RPE) could be observed and the tips of some photoreceptor outer segments adhered to the apical portions of the RPE. Cells of the outer nuclear layer were unorderly arranged and some nuclei were heavily stained. Inflammatory cells moved to the inner-limiting membrane. No obvious changes were found in the inner nuclear layer, inner plexiform layer, and ganglion cell layer. Fig. 2(a) Fundus photograph taken at 24-h post-exposure. (b) Light micrographs of the lesion. , . RPE: retinal pigment epithelium; IS/OS: inner/outer segments; ONL: outer nuclear layer; OPL: outer plexiform layer; INL: inner nuclear layer; IPL: inner plexiform layer; GCL: Ganglion cell layer; ILM: inner-limiting membrane. 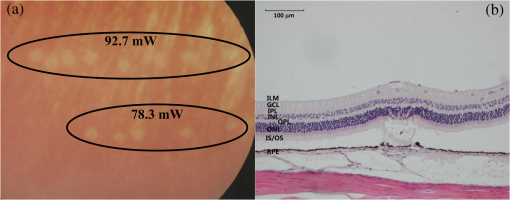 In summary, we have determined the damage threshold of chinchilla grey rabbits induced by a Vis-IR SC source and developed a theoretical method for analyzing the hazard risks of SC sources. In determining the “effective radiant exposure,” the retinal hazard spectral weighting function for humans was employed for lack of optical characteristics of rabbit. Some uncertainty may be introduced by this choice. Further studies are needed to examine the responses of non-human primates as well as the impact of exposure time. For the SC source used in the experiment, the retina is the most vulnerable part compared with other ocular media. However, for some near-infrared SC sources with a wavelength range from about 1000 nm to above 2000 nm, the retina and cornea may be damaged simultaneously. Ocular damage risks of these sources should be considered carefully and systematically. AcknowledgmentsThe authors acknowledge the financial support of Natural Science Foundation of China (Grant No. 61275194). ReferencesJ. DudleyG. GentyS. Coen,
“Supercontinuum generation in photonic crystal fiber,”
Rev. Mod. Phys., 78
(4), 1135
–1184
(2006). http://dx.doi.org/10.1103/RevModPhys.78.1135 RMPHAT 0034-6861 Google Scholar
D. J. LundP. EdsallB. E. Stuck,
“Wavelength dependence of laser-induced retinal injury,”
Proc. SPIE, 5688 383
–393
(2005). http://dx.doi.org/10.1117/12.598285 PSISDG 0277-786X Google Scholar
“ICNIRP guidelines on limits of exposure to incoherent visible and infrared radiation,”
Health Phys., 105
(1), 74
–96
(2013). http://dx.doi.org/10.1097/HP.0b013e318289a611 HLTPAO 0017-9078 Google Scholar
“ICNIRP guidelines on limits of exposure to laser radiation of wavelengths between 180 nm and ,”
Health Phys., 105
(3), 271
–295
(2013). http://dx.doi.org/10.1097/HP.0b013e3182983fd4 HLTPAO 0017-9078 Google Scholar
D. H. Slineyet al.,
“What is the meaning of threshold in laser injury experiments? Implications for human exposure limits,”
Health Phys., 82
(3), 335
–347
(2002). http://dx.doi.org/10.1097/00004032-200203000-00006 HLTPAO 0017-9078 Google Scholar
D. J. Lundet al.,
“Variation of laser-induced retinal injury thresholds with retinal irradiated area: 0.1 s duration, 514 nm exposures,”
J. Biomed. Opt., 12
(2), 024023
(2007). http://dx.doi.org/10.1117/1.2714810 JBOPFO 1083-3668 Google Scholar
|