|
|
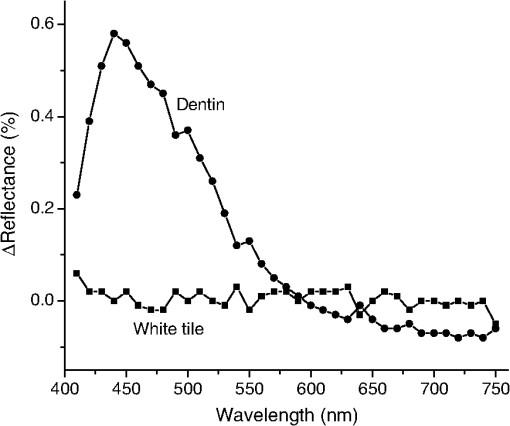
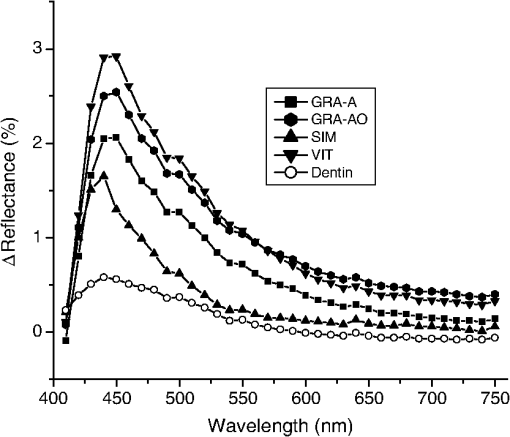
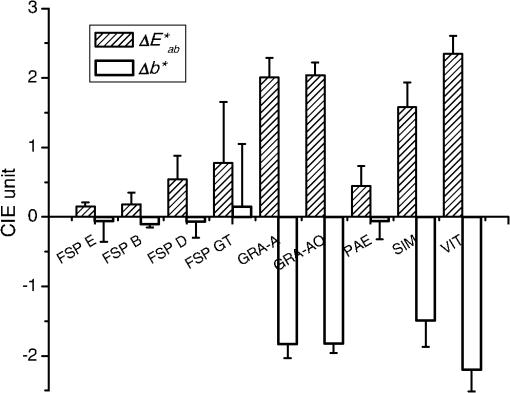
1.IntroductionIn this review article, the fluorescence properties of dental hard tissues and related esthetic restorative materials were investigated based on peer-reviewed papers. The purposes of this study were to review the fluorescence and phosphorescence of human teeth by ambient ultraviolet (UV) light that is indispensable for the esthetic rehabilitation of tooth structure, to investigate the clinically relevant fluorescence measurement methods for teeth and restorative materials and to summarize the fluorescence of human teeth and dental calculus irradiated by specific wavelength light that is used for the diagnosis of dental caries and detection of dental calculus. This article would provide an integrated view of the fluorescence properties applied in dentistry both in biology and material science fields. 2.Photoluminescence of Human TeethPhotoluminescence is emission of visible light by a substance as a result of absorption of photons, whereby radiant energy below the visible spectrum is absorbed by an object which then emits the light energy within the visible spectrum.1 Photoluminescence is divided into phosphorescence and fluorescence. Phosphorescence is defined as the induced photoluminescence that persists beyond after the cessation of the irradiation that caused it. This is in contrast to fluorescence where the photoluminescence is observed while a substance is exposed to the exciting irradiation and within after cessation.2,3 Light emitted by most fluorescent or phosphorescent substances consists of a single broad well-shaped curve, with the width and peak wavelength depending on particular fluorophore or phosphor considered.4,5 Early studies on the fluorescence and phosphorescence of human teeth involve macroscopic and microscopic techniques using UV light as a source of excitation.3 Human teeth could be made to phosphoresce for as long as 30 s with an intensity that permits their being photographed in a darkened room after the energizing irradiation was extinguished.2 As to the phosphorescence of tooth and hard tissue, phosphorescence intensities and lifetimes of calcified tissues and other biologic materials were tested.6 As results, human dentine and bone displayed nearly equal phosphorescence intensities, whereas enamel was less phosphorescent. For dentine, bone, and enamel, the experimental lifetimes of phosphorescence were . It has been also argued that phosphorescence of calcified tissues apparently stems principally from the organic moiety. However, it was also reported that the inorganic phases of bone and enamel phosphoresced, and there was a significant difference in the slopes of the phosphorescence decay curves for enamel, bone, and octacalcium phosphate.3 3.Autofluorescence of Teeth and Restorative Materials by UV Light3.1.Fluorescence of Human Teeth and Its VariationAs to the fluorescence of human teeth, two phenomena should be separately considered. One is the fluorescent emission by ambient UV light, which is important for a satisfactory esthetic restoration of teeth, and the other is fluorescent emission by a specific wavelength artificial light, such as a laser that varies by the excitation wavelength. The latter phenomenon is used for the detection of dental caries and the identification of esthetic restorative materials that are in contact with teeth.7–9 Fluorescence is a form of photoluminescence and is defined as the absorption of UV light (1 to 400 nm invisible light) by an object and its spontaneous emission in longer wavelengths (430 to 450 nm visible light).1,10 Autofluorescence is the natural emission of light by biological structures when they absorb light and is used to distinguish the light emission originating from artificially added fluorescent markers (= fluorophores).11 Autofluorescence of teeth is based on the presence of endogenous fluorophores residing in the enamel and dentine.12 Studies have shown that human teeth emit autofluorescence, although the exact chemical nature of autofluorescence remains unknown.13 Autofluorescence of human teeth by the UV light is reviewed in this section. As to the fluorescent emission of teeth by ambient UV light, it was reported in the 1910s that rabbit teeth fluoresced with a somewhat bluish intense white light. In human beings, the lens of the eye was the strongest fluorescing organ although teeth were almost equally brilliant.14,15 It was also reported that human dentine fluoresced much more brilliantly than the enamel; the white spot indicative of the beginning dental caries did not fluoresce even though unpigmented; ashed enamel did not fluoresce; and salivary calculus fluoresced quite markedly with a reddish orange color.15 Natural and many artificial light sources have UV components. When exposed to these light sources, the fluorescence of human teeth gives them the quality of vitality.16 Normal fluorescence of teeth makes an important contribution to its appearance even though it is not apparent in daylight.4 The fluorescence of sound human teeth was determined with a filter fluorometer.17 The bluish-white fluorescence of human teeth is the result of a broad emission band with a diffuse peak at 410 to 420 nm when subjected to near UV excitation of .18,19 In human teeth, fluorescence occurs primarily in dentine because of the greater amount of organic materials in dentine. Therefore, dentine fluoresced much more intensely than enamel.16 As the chroma of dentine increased, the fluorescence decreased.16,20 Enamel was also fluorescent, although it presented a smaller fluorescence index than dentine.21 As to the endogenous fluorophores in enamel and dentine, early investigations of teeth using UV excitation indicated that the light emission was from the organic matrix embedded in the inorganic calcium apatite matrix.2,6,22–24 It was also reported that the compounds causing fluorescence in human teeth were mostly organic in nature, possibly proteins, as well as the inorganic matrix.25–27 It was confirmed that fluorometric data obtained from basic hydrolysates of dentine protein were identical to those of tryptophan and tyrosine.23 Total fluorescence of calcified proteins in dentine occurred as a combination of excitation of three or more fluorescing molecules, tyrosine and tryptophan and another fluorophoric group(s).23 Investigations were undertaken into the nature of the fluorescent material in calcified tissues, which suggested that the fluorescent moiety in calcified tissues was probably derived from tyrosine.26 The emission and excitation spectra of human and bovine dental enamel and its separated organic material were determined.28 In both substances, three distinct fluorescence peaks were found in the regions 350 to 360, 405 to 410, and 440 to 450 nm. Blue fluorescence with a peak of and a width of was observed based on stationary measurements of human dentine.13 To overcome the inherent limitations of the static measurement of fluorescence, time-resolved fluorescence microscopy was used to investigate the fluorescence of human dentine.13 Fluorescent emission of human teeth may vary by the type of teeth, age, and other factors. To establish the normal range of fluorescence of human teeth, each type of tooth from the mandibular and maxillary arch were examined. As a result, fluorescence at the gingival area was significantly greater than that at the incisal area, and there was no significant difference between the maxillary and mandibular teeth nor was there any difference by gender. There was no difference in fluorescence intensity between tooth types (incisors, canine, premolar, and molar) taken from the same individual.13,29 Since enamel, dentine, and pulp suffer noticeable changes during an individual’s lifetime, fluorescence of teeth would vary by aging. Enamel becomes more mineralized with time because of the absorption of ions from saliva and foods, and dentine becomes thicker with time as pulp decreases in volume due to the deposition of secondary dentine. Additionally, dentine becomes less permeable as a result of the deposition of peritubular dentine. These changes increase the chromatic saturation of dentine while reducing its opacity.30 In natural tooth, the structural changes in enamel and dentine alter the expression of the tooth color,31 since tooth color is determined by the paths of light inside the tooth and absorption along these paths.32 When tooth is exposed to UV light, light penetrates the enamel and excites the dentine’s photosensitivity.7 Thus, age-related tooth alterations that change dentinal coloring also affect the fluorescence of tooth. It is likely that the fluorescence of dentine may be used as a reliable indicator of maturation of the human body.7 There were no differences in fluorescence intensity, decay time, or spectral profile among tooth types taken from individuals of the same age.29 The correlation between age and teeth fluorescence for individuals from different age groups was assessed via computer analysis of digital images.31 As a result, dental fluorescence decreased when comparing the age groups of 21 to 30, 31 to 40, 41 to 50, and 51 to 63 years. Dental fluorescence was correlated with age and had a similar and stable behavior from 7 to 20 years of age, reaching its maximum expected value at the age of 26.5 years and thereafter decreasing. However, it was reported that the intensity of the fluorescence increased, whereas the decay time decreased with aging based on a nanosecond time-resolved fluorescence microphotometer.29 It was also reported that increases in fluorescence intensity were found to be dependent upon age regardless of tooth type or gender.13 Further studies for the age-related variations in fluorescence of teeth should be performed. 3.2.Fluorescence of Dental Restorative Materials and Its SignificanceThe ultimate esthetic dentistry takes into account the conservation of healthy tooth structures integrated with biologic and long-term functional requirements. Therefore, materials and techniques that address these inseparable issues are necessary for true excellence.33 Closely matching natural teeth with an artificial restoration can be one of the most challenging procedures in restorative dentistry. It is only possible to duplicate in restorative materials what has been distinguished, understood, and communicated in the shade matching process of the natural dentition.34 In this sense, fluorescence, opalescence, and translucency are critical for dental restorative materials to mimic the optical properties and appearance of natural teeth.35 Ideally, a restorative material should have fluorescence similar to that of natural teeth. Fluorescence needs to be tested in addition to color, as the two characteristics are uncorrelated. In fact, fluorescence is becoming more important due to the widespread use of artificial lighting with blue or UV contributions.36 In 1977, it was reported that the basic components of dental anterior restorative materials did not fluoresce, but this quality could be achieved by the addition of fluorescent components.4 The fluorescence spectra of dental porcelains and acrylic resins were published in 1978.18 Natural teeth and several commercial dental resin composites emit a strong blue fluorescence when exposed to UV light, which makes teeth whiter and brighter in daylight.37 Resin composites with a higher fluorescence can be added strategically to restorations to increase the amount of light returning to the viewer, block out discolorations, and lower the chroma. This is especially beneficial with high-value shades placed within layers of resin composite for dentine, as it can make the value higher without negatively affecting the translucency.34 Before discussing the harmonization or differentiation of fluorescence between natural teeth and restorative materials, several methodological aspects for clinically relevant fluorescence measurements for dentistry were reviewed. The fluorescence of human dentine and dental resin composites were determined with a color-measuring spectrophotometer.38 Spectral reflectance was measured over a white standard tile according to the Commission Internationale de l’Eclairage (CIE) LAB color scale relative to the CIE standard illuminant D65. A UV filter was inserted or removed to exclude or include the UV component of the illumination. From the spectral reflectance values, the subtraction spectrum was calculated by the inclusion and exclusion of the UV component, and the color difference by the UV component was defined as the fluorescence parameter (). The color difference between the pair was calculated as , in which subscripts and indicated UV included and excluded, respectively.39 As a result, dentine showed a fluorescence peak around 440 to 450 nm (Fig. 1). Three of the five commercial resin composites investigated showed fluorescence peaks, with a peak wavelength of 440 to 450 nm (Fig. 2). The peak height and peak area varied by brand. The fluorescence parameter was 1.6 to 2.4, and the difference in the CIE value () by the inclusion or exclusion of the UV component was from to in resin composites that showed fluorescence peaks (Fig. 3). The differences in color and color attributes, such as lightness, chroma, and hue, of dental resin composites created by varying the amount of the UV component of a pulsed-xenon source that was conditioned to approximate the CIE standard illuminant D65 were determined.40 The color of specimens was measured relative to three illuminations, which had the same spectral power distribution of the CIE standard illuminant D65 in the visible range, but a different UV component. D65 indicated the illumination in which the UV component was adjusted to the CIE standard illuminant D65 using a UV adjustment tile. UV-EXC indicated the illumination in which the UV component of the source was excluded with a UV filter. UV-INC indicated the illumination in which the UV component was included. As a result, the fluorescence parameter by the amount of UV component ranged between 0.3 and 1.4 for D65 and UV-EXC, between 0.3 and 0.5 for D65 and UV-INC, and between 0.2 and 1.6 for UV-EXC and UV-INC. Fluorescence properties of indirect and direct resin composites before and after polymerization were determined.41 Resin materials were packed into a mold (BEC condition) and polymerized with a light-polymerization unit (CWL). Secondary polymerization (CIC) was performed for indirect composites. The fluorescence parameter was measured in the BEC, CWL, and CIC conditions. The mean fluorescence parameter value for an indirect resin composite brand was 2.5 before polymerization, which changed to 0.7 after polymerization (Fig. 4). The fluorescence properties of resin materials varied depending on the material, shade group, and polymerization. Fig. 4Fluorescence parameter values before polymerization (BEC), after polymerization with a polymerization light (CWL), and after polymerization in the polymerization chamber (CIC) of an indirect resin composite brand by the shade. 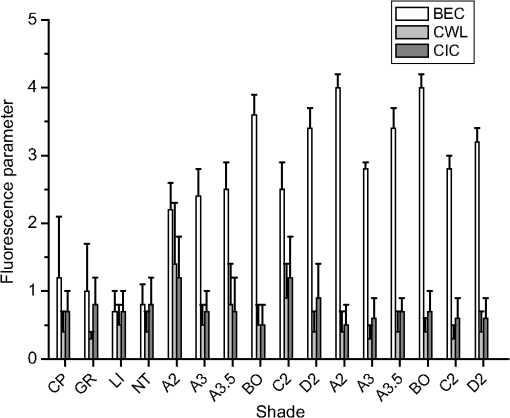 Daylight illumination varies during the day due to weather or other conditions that change the amount of the UV component in daylight. The level of the UV component in daylight may influence the color of fluorescent resin composites.42 Spectral reflectance and the colors of four brands of resin composites were measured relative to the UV adjusted illuminant D65. A UV filter of a spectrophotometer was adjusted to change the UV component of the illuminant D65. From the spectral reflectance values, subtraction spectra between the spectra in UV-included conditions (20, 40, 60, 80, and 100%) and that in the 0% UV condition of the illuminant D65 were calculated. The fluorescence parameter between each of the UV-included conditions and the 0% UV condition was also calculated. Peak height based on subtraction spectra was in the range of 0.4 to 2.4. Fluorescence parameter ( to 2.7) was influenced by the included percentage of the UV component and the brand of composite resin. The effects of a fluorescent whitening agent with a concentration of 0.01 to 0.1% on the fluorescent emission of experimental resin composites were also determined.43 As a result, the concentration of the fluorescent whitening agent influenced the fluorescent peak heights and areas and the fluorescence peak height and area were also influenced by the resin matrix. The changes in the fluorescence parameter of dental resin composite, glass-ionomer, resin-modified glass-ionomer, and compomer before and after accelerated aging () were determined.44 As a result, aging and the type of material significantly influenced the fluorescence parameter values. Regarding the fluorescence of teeth and dental restorative materials, two aspects, the esthetic reproduction of the tooth structure with restorative materials and the reverse differentiation of restored materials to remove or to identify forensic use, should be considered. As to the esthetic reproduction of the tooth structure, the optical characteristics of the natural teeth are essential to masking the restoration and are determined by the interaction of light and dental substrates with varying degrees of translucency and opacity.45 The fluorescence of restorative materials allows for a closer representation to that of human enamel and dentine, and provides a whiter and brighter aspect, minimizing the artificial gray aspect of having no fluorescent materials present. Different light sources emit UV radiation at distinct intensities, which can result in varied patterns of tooth and restorative material fluorescence.8 The optical integration and fluorescence of dental restorative materials was evaluated.8 For this, resin-based materials were used to consecutively restore 10 extracted incisors, and the results indicated that optical integration scores varied by the type of material. The fluorescence of dental resin composites and ceramics were studied with coffee, tea, red wine, and distilled water (control) as staining drinks.36 Time-resolved fluorescence spectra were recorded using a laser nanosecond spectrofluorometer. The materials tested demonstrated significantly different initial fluorescence intensities. Upon exposure to staining drinks, fluorescence became weaker by up to 40%. Therefore, it is important to further improve the color and luminescence stability of dental materials.36 As to the differentiation or identification of restored materials by fluorescence difference, it may be difficult to recognize resin composite restorations that are correctly shade-matched and well-placed by visual and tactile inspection alone, which can make the replacement of an existing resin restoration challenging.46 Many resin composites fluoresce under UV light, which can help dentists to detect resin materials.46 The presence of tooth-colored resin fillings in the dentition presents a challenge to the forensic odontologist, as detection of the fillings can be difficult both visually and radiographically.7 UV inspection is of interest because enamel, dentine, and dental materials all have differing fluorescent properties when illuminated by UV light.7 There have been reports that fluorescence can be used as a tool to identify a dental restorative material, distinguish it from natural tooth tissue, and allow it to be examined after staining.28,47,48 Differentiation of resin composite restorations from teeth using fluorescent emission was investigated as basic research for the visual detection of resin-filled teeth in mass dental health examinations.49 For this, fluorescence spectra were taken from extracted human maxillary central incisors and 12 types of resin composites via excitation using light with wavelengths of 400 to 500 nm (400, 430, 450, and 470 nm). The fluorescent images were taken based on spectroscopic results, which confirmed the discrimination between the resin part and the tooth in the resin-filled tooth. Historically, UV inspection lights of the tube or lamp type have been large and difficult to use for dental inspection.7 In recent years, small light-emitting diode (LED) flashlights emitting at specific wavelengths in the UV range have been developed. Practical use and comparison of the LED flashlights revealed that the most useful excitation wavelengths for resin detection were in the UV A range (365 and 380 nm). Porcelain restorations and resin composite fillings exhibited different responses to these two wavelengths, thus the use of both is recommended for forensic dental inspection. To explore a technique that utilizes a UV LED to cause composite resin to fluoresce,46 a UV/visible light spectrofluorometer was used to measure fluorescence excitation and emission maxima of varied resin composite brands, dentine, and enamel. Results from this study indicated that the optimal excitation wavelength was 385 to 395 nm, while 460 nm was determined to be the mean emission maxima. Based on the results of this study, it was concluded that the use of UV illumination could be a useful technique for determining whether or not a resin composite had been removed completely. Differentiation of porcelain from tooth using fluorescent emission was investigated for the visual detection of porcelain-restored teeth in mass dental health examinations.47 The fluorescence spectra were taken from the extracted human maxillary central incisors and five types of porcelain by excitation using light of 380 to 470 nm. As a result, there was a clear difference in fluorescence intensity between tooth and porcelain using excitations longer than 400 nm. Therefore, tooth and porcelain could be successfully distinguished on an image photographed by fluorescent light. Fluorescent characteristics of silicate cements, acrylic resins, and resin composites were compared with natural teeth when specimens were submitted to UV radiation.4 The fluorescent light spectrum was determined using a UV light source of 365 nm and a spectrophotometer with a fluorescence attachment. Although some of the materials exhibited fluorescence under UV light, there were major differences between them, and one of the silicate cements was shown to have a high intensity at 460 and 525 nm.4 4.Fluorescence Properties of Dental Caries and Dental Calculus4.1.Wavelength-Dependent Fluorescence of TeethAs the emphasis shifts from damage mitigation to disease prevention or reversal of early disease in the oral cavity, the need for sensitive and accurate detection and diagnostic tools become more important.50 Many novel and emergent optical diagnostic modalities for the oral cavity are becoming available with a variety of desirable attributes, including (1) noninvasiveness, (2) absence of ionizing radiation, (3) patient-friendliness, (4) real-time information, (5) repeatability, and (6) high-resolution surface and subsurface images.50 Fluorescence detection is a noncontact, nondestructive probing technique which has received increasing attention due to its high sensitivity and specificity.51 In this section, fluorescence emitted by specific wavelength light of sound and caries tooth structures and dental calculus and the application of this property to the clinical application for the diagnosis of dental caries and the determination of the extent of surgical removal of caries-affected tooth tissue was considered. For caries diagnosis, wavelength-dependent fluorescence properties are used instead of fluorescent emission under ambient lights that contain UV light. It is well known that dental enamel and dentine exhibit laser-induced fluorescence. The fluorescence spectra of sound teeth have been reported to be dependent on the excitation wavelength.52 As to the spectra of fluorescent emission from cross-sectioned enamel samples subjected to a range of excitation wavelengths (380 to 580 nm), a redshift of the peak emission wavelength was observed as the excitation moved to a longer wavelength.52 4.2.Fluorescence of Dental CariesCaries lesions in dental hard tissues fluoresce when exposed to light of a certain wavelength, whereas sound tissues do not, and this can be used as an in vitro histological marker for dental caries.53 As to the fluorescence spectra by a specific wavelength for caries detection, varied wavelengths were studied, such as 488,24,54,55 407,12 400 to 420,52 337,56 and 405, 444, and 532 nm.9 Fluorescence spectra of enamel and dentine illuminated with laser light of wavelengths of 337, 488, 515, and 633 nm were recorded.24 In both tissues, the fluorescence obtained by illumination at 337 nm (UV light) had a peak at , and illumination at 488 nm produced fluorescence with a peak at . Compared to intact enamel, the fluorescence from enamel with initial carious lesions was of lower intensity and had a slight redshift. Therefore, it was concluded that illumination at 488 nm was the most suitable wavelength of those investigated for the detection of initial carious lesions. The associations between the fluorescence distribution in carious dentine (excited by 488-nm laser) and color, mineral density, bacterial distribution, and microhardness of the lesions in vitro were reported.54 This study indicated that the fluorescence signal might be elicited from bacterial molecules or denatured collagen breakdown products, thus highlighting the outermost, softer caries-infected dentine layer requiring clinical excavation.54 The relationship between the microhardness of carious dentine and its native fluorescence was investigated.55 Carious molar teeth were sectioned through natural lesions and the Knoop hardness number (KHN) of the cut surfaces was recorded at regular intervals. Confocal fiber-optic micro-endoscopic examination of the carious dentine and the sound dentine was carried out with an excitation wavelength of 488 nm. The data analysis indicated that the fluorescence signals increased significantly when the microhardness of dentine dropped below 25 KHN. Therefore, the fluorescent signal intensity could produce an objective and reproducible correlation to the microhardness of carious dentine. The spectral fluorescence characteristics of dental caries were studied.12 A wide range of carious lesions revealed characteristic emission of endogenous fluorophores with strong fluorescence bands in the red spectral region when excited with 407 nm. Healthy hard dental tissue exhibited no emission bands in the red. The fluorescence spectra, fluorescence excitation spectra as well as the reflectance spectra of carious lesions, were found to be typical for fluorescent porphyrins, mainly protoporphyrin IX.12 A possible source of these porphyrins within carious tissues was bacterial biosynthesis; therefore, noninvasive sensitive in vivo caries detection by means of appropriate excitation sources and porphyrin fluorescence detectors should be possible. Emission spectra from noncavitated enamel caries with different degrees of discoloration under a wide range of excitation wavelengths were compared using a fluorescence spectrophotometer at excitation wavelengths from 360 up to 580 nm in steps of 20 nm.52 As a result, emission spectra of all types of carious lesions were shifted toward longer wavelengths (redshift) when compared to the spectra of the corresponding sound enamel. The redshift was significantly highest for dark brown spot lesions and lowest for white spot lesions. Distinct fluorescence bands within 600 to 700 nm typical for porphyrin compounds were strongest for excitation wavelengths from 400 to 420 nm and were present in most of the lesions investigated. Laser-induced fluorescence spectra of teeth irradiated by a 337-nm laser were measured during in vitro caries formation.56 Spectra obtained from sound teeth consist of an intensive maximum at 480 to 500 nm and a secondary maximum at 430 to 450 nm. In the process of caries formation, an increase in the intensity at 430 to 450 nm and the appearance of two maxima in the red spectral region at 590 to 650 nm were observed. The intensity increase at 430 to 450 nm was related to the tooth demineralization and bacteria presence and their metabolism products induced an increase in the absorption in the UV-blue spectral region at 350 to 420 nm and the appearance of a fluorescence signal in the long-wave spectral region at 590 to 650 nm. Fluorescence spectra by artificial single wavelength light at 405, 444, and 532 nm were recorded in vitro from human dentine, enamel, and whole teeth.9 The emission spectra exhibited a broad peak shifted by to 75 nm from the excitation wavelength, and the shape of the spectra remained similar regardless of the excitation wavelength. The maximum of the fluorescence spectra also exhibited a redshift that depended upon the laser excitation wavelength. A redshift of the excitation wavelength led to a corresponding redshift in the wavelength of maximum autofluorescence. As the excitation wavelength was moved from short wavelengths (405 nm) to longer wavelengths (532 nm), the peak of the observed emission shifted from 480 to 579 nm, respectively. Quantitative light-induced fluorescence (QLF; Inspektor Dental Care, Netherlands) uses fluorescence induced by multiwavelength excitation at 290 to 450 nm to measure mineral loss in enamel and dentine. This device provides color-coded images of the target tissues. Sound tooth structures fluoresce and carious tooth structures appear dark.50 QLF can detect about twice as many demineralized precavitated enamel areas compared to a conventional visual examination or any other caries detection instrument.50 QLF methodology could detect, within three- and six-month periods, a difference in remineralization between fluoride-containing and non-fluoride-containing dentifrices.57 The demineralization and remineralization of intact root surface and cavitated caries lesions were determined using a QLF system, and the QLF system was able to detect early root surface caries lesions in vivo.58 It was determined whether or not QLF parameters [area (; ), fluorescence loss (; %), and ()] could predict lesion progression.59 QLF , , and increased at a faster rate for surfaces that progressed than for surfaces that did not progress. Therefore, it was concluded that faster changes in QLF variables can indicate lesion progression toward cavitation and can be more clinically relevant than actual QLF values. It was determined whether QLF parameters, and , were appropriate for aiding diagnosis and clinical decision making of early occlusal mineral loss by comparing QLF analysis with actual restorative management.60 DIAGNOdent (DD; KavoDental GmbH, Germany) uses a laser to excite fluorescence from pigments in carious tooth structure.61 The correlation between DD readings and the extent of incipient occlusal caries as measured by the volume of tooth preparation in vitro was evaluated.62 The Pearson correlation for preparation volume and DD reading measurements was low (correlation coefficient: ). Within the limitations of this study, DD readings did not correlate well with the extent of carious tooth structure in incipient occlusal caries. The distance and the presence of tooth structure between the carious lesion and the instrument’s tip reduced DD readings. These results indicated that anatomic factors interfere with the device’s ability to assess occlusal caries. Therefore, DD readings should not be relied on when making diagnostic decisions.61 As to the caries removal by fluorescence change, it has been reported that the fluorescence of carious dentine is a microscopic marker for tissue requiring surgical excavation.54 The removal of infected, demineralized dentine with a laser feedback mechanism (KaVo DIAGNOdent) was evaluated.53 Complete removal of demineralized tissue occurred under feedback control at values of 7 and 8, and the removal of demineralized dentine was incomplete at greater values. 4.3.Fluorescence of Dental CalculusSubgingival calculus has been recognized as a major cause of periodontitis, which is one of the main chronic infectious diseases of oral cavities and a principal cause of tooth loss in humans.63 Successful periodontal therapy requires sensitive techniques to discriminate dental calculus from healthy teeth.51 Therefore, the possibility of detecting subgingival calculus should be evaluated to control complete calculus removal after scaling and root planing.64 In 1953, it was noted that dental calculus on teeth surfaces showed reddish-orange fluorescence under the UV light.10 A report on the detection and removal of dental calculus with the aid of fluorescent emission using varied wavelengths and instruments was made.64 The emission spectra from supra- and subgingival calculus under a wide range of excitation wavelengths were investigated.65 This fluorescent emission was strongest for excitation wavelengths from 400 to 420 nm, and human dental calculus could clearly be differentiated from clean root surfaces by emission spectrophotometry. It was also assumed that the characteristic fluorescent emission of dental calculus might be due to a variety of porphyrin derivatives. Fluorescence was measured at various excitation and emission wavelength settings for sound dentine and enamel, subgingival calculus, and root caries.66 Subgingival calculus and root caries showed a characteristic 700 nm emission when excited at 635 nm or a 720 nm emission when excited at 655 nm; sound dentine or enamel, however, did not. Therefore, the autofluorescence method employing excitation of 633 to 635 nm was found to be a powerful tool for detecting subgingival calculus and root caries. The use of fluorescent emission induced by the diode laser radiation () for the detection of subgingival calculus was evaluated,67 which indicated that subgingival calculus can be reliably detected on extracted teeth because of considerably higher amounts of fluorescence in subgingival calculus than in cementum. To investigate the laser-fluorescence effects on tooth root surfaces, extracted human teeth partially covered with calculus were irradiated by light from a diode laser ().65 This study indicated that laser-fluorescence values on the root surface were strongly correlated to the presence of calculus. Therefore, the fluorescence effect can basically be used to develop a new detecting system for subgingival calculus in periodontal pockets. Three devices developed to assist in detecting small deposits of subgingival calculus, all of which use visible red light-induced fluorescence (), were compared. In each system, near-infrared fluorescence emissions from bacterial products are collected using rigid sapphire tips which are placed inside periodontal pockets and slid along the root surfaces of teeth.68 These results indicate that while visible red laser-fluorescence systems vary somewhat in performance, their laser-fluorescence readings provide a useful estimation of the volume of subgingival calculus deposits present on teeth. A subgingival calculus detection system employing autofluorescence imaging based on two-photon time-correlated fluorescence technique was developed.69 The detection of subgingival calculus employing a multiphoton autofluorescence imaging method was characterized in comparison with a one-photon confocal fluorescence imaging technique.63 The multiphoton fluorescence technology perceived the tissue-covered subgingival calculus that could not be observed by the one-photon confocal fluorescence method. The laser-induced calculus fluorescence phenomenon and the calculus detection devices were reviewed and the clinical relevance of using commercialized calculus detection devices in periodontal treatment was determined.70 Very few studies demonstrated that the Er:YAG laser debridement, when performed with automatic calculus detection, could lead to improvements at the clinical level. Although preliminary data were encouraging, there was a lack of scientific data concerning the calculus detection devices. The removal of subgingival calculus and dental hard tissues depending on the threshold level of a fluorescence feedback-controlled Er:YAG laser was evaluated.71 The amount of residual calculus following laser irradiation depends on the fluorescence threshold level for a feedback-controlled Er:YAG laser. The possibility of detecting subgingival calculus with an LED-based optical probe was assessed.72 The optical probe offers the possibility of subgingival calculus detection and may, therefore, be suited to determine the endpoint of root surface instrumentation during nonsurgical periodontal therapy. Human teeth with sub- and supragingival calculus and healthy teeth were illuminated by a focused blue LED light source of 405 nm, and the fluorescence spectra of each tooth were confirmed by clinical and histological findings. The results indicated that this method enabled cost-effective and reliable calculus detection, and can be further developed for imaging applications.51 A fluorescence-based procedure to enable real-time detection and quantification of dental calculus was developed.51 5.ConclusionsAs to the fluorescence of human teeth, two phenomena should be separately considered: one is the fluorescent emission by ambient UV light applied for esthetic restoration of teeth and the other is fluorescent emission by a specific wavelength light used for the detection of dental caries and the identification of restorative materials. When human teeth were exposed to UV sources, fluorescence with a peak of 440 nm was observed. A restorative material should have a fluorescence similar to that of natural tooth. A relevant measurement method was defined. Several methods for the diagnosis of dental caries and detection of dental calculus were developed based on the fluorescence spectra emitted at specific wavelength(s). Since fluorescent properties of dental hard tissues are used in diverse fields of clinical practice, these properties should be investigated further embracing newly introduced optical techniques, such as spectral imaging that integrates conventional imaging and spectroscopy to get both spatial and spectral information from an object73 or hyperspectral imaging that acquires a three-dimensional dataset called a hypercube with two spatial dimensions and one spectral dimension.74 ReferencesH. J. Wilson,
“Restorative materials and ultra-violet radiation,”
Br. Dent. J., 126
(8), 345
–346
(1969). BDJOAJ 0007-0610 Google Scholar
J. Wisotzky,
“Effects of neo-tetrazolium chloride of the phosphorescence of teeth,”
J. Dent. Res., 43
(5), 659
–668
(1964). http://dx.doi.org/10.1177/00220345640430050701 JDREAF 0022-0345 Google Scholar
P. D. Frazier, D. W. Engen and S. K. Scamack,
“X-ray induced light emission from enamel, bone, and other calcium phosphate materials,”
J. Dent. Res., 46
(4), 731
–735
(1967). http://dx.doi.org/10.1177/00220345670460041601 JDREAF 0022-0345 Google Scholar
H. Panzeri, L. T. Fernandes and C. J. Minelli,
“Spectral fluorescence of direct anterior restorative materials,”
Aust. Dent. J., 22
(6), 458
–461
(1977). http://dx.doi.org/10.1111/adj.1977.22.issue-6 ADEJA2 0045-0421 Google Scholar
E. Drakaki et al.,
“Laser-induced fluorescence made simple: implications for the diagnosis and follow-up monitoring of basal cell carcinoma,”
J. Biomed. Opt., 19
(3), 030901
(2014). http://dx.doi.org/10.1117/1.JBO.19.3.030901 JBOPFO 1083-3668 Google Scholar
K. C. Hoerman and S. A. Mancewics,
“Phosphorescence of calcified tissues,”
Arch. Oral Biol., 9
(5), 517
–534
(1964). http://dx.doi.org/10.1016/0003-9969(64)90016-0 AOBIAR 0003-9969 Google Scholar
A. S. Hermanson et al.,
“Ultraviolet illumination as an adjunctive aid in dental inspection,”
J. Forensic Sci., 53
(2), 408
–411
(2008). http://dx.doi.org/10.1111/j.1556-4029.2008.00657.x JFSCAS 0022-1198 Google Scholar
D. Lefever et al.,
“Optical integration and fluorescence: a comparison among restorative materials with spectrophotometric analysis,”
Quintessence Int., 41
(10), 837
–844
(2010). 0033-6572 Google Scholar
L. Zhang, L. Y. Nelson and E. J. Seibel,
“Red-shifted fluorescence of sound dental hard tissue,”
J. Biomed. Opt., 16
(7), 071411
(2011). http://dx.doi.org/10.1117/1.3606572 JBOPFO 1083-3668 Google Scholar
R. L. Hartles and A. G. Leaver,
“The fluorescence of teeth under ultraviolet irradiation,”
Biochem. J., 54
(4), 632
–638
(1953). BIJOAK 0264-6021 Google Scholar
M. Monici,
“Cell and tissue autofluorescence research and diagnostic applications,”
Biotechnol. Annu. Rev., 11 227
–256
(2005). http://dx.doi.org/10.1016/S1387-2656(05)11007-2 BAREFD 1387-2656 Google Scholar
K. König, G. Flemming and R. Hibst,
“Laser-induced autofluorescence spectroscopy of dental caries,”
Cell. Mol. Biol., 44
(8), 1293
–1300
(1998). CMBID4 0145-5680 Google Scholar
H. Matsumoto, S. Kitamura and T. Araki,
“Applications of fluorescence microscopy to studies of dental hard tissue,”
Front. Med. Biol. Eng., 10
(4), 269
–284
(2001). http://dx.doi.org/10.1163/156855700750265459 FMBEEQ Google Scholar
H. Stübel,
“Die Fluoreszenz tierischer Gewebe in ultraviolettem Licht,”
Arch. Ges. Physiol., 142
(1), 1
–14
(1911). http://dx.doi.org/10.1007/BF01680690 Google Scholar
H. C. Benedict,
“A note on the fluorescence of teeth in ultraviolet rays,”
Science, 67
(1739), 442
(1928). http://dx.doi.org/10.1126/science.67.1739.442 SCIEAS 0036-8075 Google Scholar
R. Winter,
“Visualizing the natural dentition,”
J. Esthet. Dent., 5
(3), 103
–117
(1993). http://dx.doi.org/10.1111/jerd.1993.5.issue-3 1040-1466 Google Scholar
J. B. Hall, J. J. Hefferren and N. H. Olsen,
“Study of fluorescent characteristics of extracted human teeth by use of a clinical fluorometer,”
J. Dent. Res., 49
(6), 1431
–1436
(1970). http://dx.doi.org/10.1177/00220345700490064601 JDREAF 0022-0345 Google Scholar
W. T. Wozniak and B. K. Moore,
“Luminescence spectra of dental porcelains,”
J. Dent. Res., 57
(11–12), 971
–974
(1978). http://dx.doi.org/10.1177/00220345780570111201 JDREAF 0022-0345 Google Scholar
G. A. Ecker et al.,
“Effect of repeated firing on fluorescence of porcelain-fused-to-metal porcelains,”
J. Prosthet. Dent., 54
(2), 207
–214
(1985). http://dx.doi.org/10.1016/0022-3913(85)90290-2 JPDEAT 0022-3913 Google Scholar
E. McLaren,
“The 3D-Master shade-matching system and the skeleton buildup technique: science meets art and intuition,”
Quintessence Dent. Technol., 22
(1), 55
–68
(1999). Google Scholar
H. Tsuda, J. Ruben and J. Arends,
“Raman spectra of human dentin mineral,”
Eur. J. Oral Sci., 104
(2), 123
–131
(1996). http://dx.doi.org/10.1111/eos.1996.104.issue-2 EJOSFY 0909-8836 Google Scholar
G. Dickson et al.,
“Fluorescence of teeth; a means of investigating their structure,”
J. Am. Dent. Assoc., 45
(6), 661
–667
(1952). http://dx.doi.org/10.14219/jada.archive.1952.0234 0002-8177 Google Scholar
K. C. Hoerman and S. A. Mancewics,
“Fluorometric demonstration of tryptophan in dentin and bone protein,”
J. Dent. Res., 43
(2), 276
–280
(1964). http://dx.doi.org/10.1177/00220345640430021601 JDREAF 0022-0345 Google Scholar
F. Sundström et al.,
“Laser-induced fluorescence from sound and carious tooth substance: spectroscopic studies,”
Swed. Dent. J., 9
(2), 71
–80
(1985). SDJOD5 Google Scholar
H. J. Horsley,
“Isolation of fluorescent materials present in calcified tissue,”
J. Dent. Res., 46
(1), 106
(1967). JDREAF 0022-0345 Google Scholar
C. A. McDevitt and W. G. Armstrong,
“Investigations into the nature of the fluorescent material in calcified tissues,”
J. Dent. Res., 48
(6), 1108
(1969). JDREAF 0022-0345 Google Scholar
J. J. Hefferren et al.,
“Phosphorescence of enamel treated with stannous salts,”
J. Dent. Res., 46
(6), 1368
–1371
(1967). http://dx.doi.org/10.1177/00220345670460063801 JDREAF 0022-0345 Google Scholar
D. Spitzer and J. J. Bosch,
“The total luminescence of bovine and human dental enamel,”
Calcif. Tissue Res., 20
(1), 201
–208
(1976). http://dx.doi.org/10.1007/BF02546408 CATRBZ 0008-0594 Google Scholar
H. Matsumoto, S. Kitamura and T. Araki,
“Autofluorescence in human dentine in relation to age, tooth type and temperature measured by nanosecond time-resolved fluorescence microscopy,”
Arch. Oral Biol., 44
(4), 309
–318
(1999). http://dx.doi.org/10.1016/S0003-9969(98)00126-5 AOBIAR 0003-9969 Google Scholar
L. N. Baratieri, E. Araujo and S. MonteiroJr.,
“Color in natural teeth and direct resin composite restorations: essential aspects,”
Eur. J. Esthet. Dent., 2
(2), 172
–186
(2007). 1862-0612 Google Scholar
R. D. da Silva et al.,
“Dental fluorescence: potential forensic use,”
Forensic Sci. Int., 231
(1–3), 167
–171
(2013). http://dx.doi.org/10.1016/j.forsciint.2013.05.001 FSINDR 0379-0738 Google Scholar
J. J. ten Bosch and J. C. Coops,
“Tooth color and reflectance as related to light scattering and enamel hardness,”
J. Dent. Res., 74
(1), 374
–380
(1995). http://dx.doi.org/10.1177/00220345950740011401 JDREAF 0022-0345 Google Scholar
E. A. McLaren,
“Luminescent veneers,”
J. Esthet. Dent., 9
(1), 3
–12
(1997). http://dx.doi.org/10.1111/jerd.1997.9.issue-1 1040-1466 Google Scholar
J. Fondriest,
“Shade matching in restorative dentistry: the science and strategies,”
Int. J. Periodontics Restorative Dent., 23
(5), 467
–479
(2003). http://dx.doi.org/10.1016/j.prosdent.2004.03.015 0198-7569 Google Scholar
F. Komine et al.,
“A modified layering technique to enhance fluorescence in glass-infiltrated aluminum oxide ceramic restorations: case report,”
Quintessence Int., 39
(1), 11
–16
(2008). 0033-6572 Google Scholar
M. Gawriołek et al.,
“Color and luminescence stability of selected dental materials in vitro,”
J. Prosthodont., 21
(2), 112
–122
(2012). http://dx.doi.org/10.1111/jopr.2011.21.issue-2 JPORCN 1059-941X Google Scholar
Y. K. Lee, H. Lu and J. M. Powers,
“Effect of surface sealant and staining on the fluorescence of resin composites,”
J. Prosthet. Dent., 93
(3), 260
–266
(2005). http://dx.doi.org/10.1016/j.prosdent.2004.12.017 JPDEAT 0022-3913 Google Scholar
Y. K. Lee, H. Lu and J. M. Powers,
“Fluorescence of layered resin composites,”
J. Esthet. Restor. Dent., 17
(2), 93
–101
(2005). http://dx.doi.org/10.1111/jerd.2005.17.issue-2 1496-4155 Google Scholar
“Colorimetry,”
(2004). Google Scholar
H. Lu et al.,
“Influence of the amount of UV component in daylight simulator on the color of dental composite resins,”
J. Prosthet. Dent., 96
(5), 322
–327
(2006). http://dx.doi.org/10.1016/j.prosdent.2006.08.007 JPDEAT 0022-3913 Google Scholar
S. H. Song et al.,
“Opalescence and fluorescence properties of indirect and direct resin materials,”
Acta Odontol. Scand., 66
(4), 236
–242
(2008). http://dx.doi.org/10.1080/00016350802208414 AOSCAQ 0001-6357 Google Scholar
Y. K. Lee, J. H. Kim and J. S. Ahn,
“Influence of the changes in the UV component of illumination on the color of composite resins,”
J. Prosthet. Dent., 97
(6), 375
–380
(2007). http://dx.doi.org/10.1016/S0022-3913(07)60026-2 JPDEAT 0022-3913 Google Scholar
M. Y. Park, Y. K. Lee and B. S. Lim,
“Influence of fluorescent whitening agent on the fluorescent emission of resin composites,”
Dent. Mater., 23
(6), 731
–735
(2007). http://dx.doi.org/10.1016/j.dental.2006.06.028 DEMAEP 0109-5641 Google Scholar
Y. K. Lee and J. M. Powers,
“Influence of opalescence and fluorescence properties on the light transmittance of resin composite as a function of wavelength,”
Am. J. Dent., 19
(5), 283
–288
(2006). 0894-8275 Google Scholar
R. F. Mondelli et al.,
“Challenges of restoring an anterior maxillary tooth: the impact of fluorescence and the mock-up approach,”
Quintessence Int., 43
(10), 859
–862
(2012). 0033-6572 Google Scholar
M. A. Bush et al.,
“The use of ultraviolet LED illumination for composite resin removal: an in vitro study,”
Gen. Dent., 58
(5), e214
–e218
(2010). 0363-6771 Google Scholar
K. Tani et al.,
“Fluorescent properties of porcelain-restored teeth and their discrimination,”
Mater. Trans., 45
(4), 1010
–1014
(2004). http://dx.doi.org/10.2320/matertrans.45.1010 MTJIEY 0916-1821 Google Scholar
A. Mazur-Koczorowska et al.,
“Luminescence of selected dental composites in vitro,”
Dent. Mater., 24
(10), 1329
–1335
(2008). http://dx.doi.org/10.1016/j.dental.2008.02.014 DEMAEP 0109-5641 Google Scholar
K. Tani et al.,
“Discrimination between composite resin and teeth using fluorescence properties,”
Dent. Mater. J., 22
(4), 569
–580
(2003). http://dx.doi.org/10.4012/dmj.22.569 DMJOD5 Google Scholar
P. Wilder-Smith et al.,
“Optical diagnostics in the oral cavity: an overview,”
Oral Dis., 16
(8), 717
–728
(2010). http://dx.doi.org/10.1111/odi.2010.16.issue-8 1354-523X Google Scholar
Y. L. Qin et al.,
“Real-time detection of dental calculus by blue-LED-induced fluorescence spectroscopy,”
J. Photochem. Photobiol. B, 87
(2), 88
–94
(2007). http://dx.doi.org/10.1016/j.jphotobiol.2007.03.002 JPPBEG 1011-1344 Google Scholar
W. Buchalla,
“Comparative fluorescence spectroscopy shows differences in noncavitated enamel lesions,”
Caries Res., 39
(2), 150
–156
(2005). http://dx.doi.org/10.1159/000083162 CAREBK 0008-6568 Google Scholar
D. R. Schwass et al.,
“Evaluating the efficiency of caries removal using an Er:YAG laser driven by fluorescence feedback control,”
Arch. Oral Biol., 58
(6), 603
–610
(2013). http://dx.doi.org/10.1016/j.archoralbio.2012.09.017 AOBIAR 0003-9969 Google Scholar
A. Banerjee et al.,
“A confocal microscopic study relating the auto-fluorescence of carious dentine to its microhardness,”
Br. Dent. J., 187
(4), 206
–210
(1999). BDJOAJ 0007-0610 Google Scholar
A. Banerjee et al.,
“A confocal micro-endoscopic investigation of the relationship between the microhardness of carious dentine and its autofluorescence,”
Eur. J. Oral Sci., 118
(1), 75
–79
(2010). http://dx.doi.org/10.1111/eos.2010.118.issue-1 EJOSFY 0909-8836 Google Scholar
E. Borisova, T. Uzunov and L. Avramov,
“Laser-induced autofluorescence study of caries model in vitro,”
Lasers Med. Sci., 21
(1), 34
–41
(2006). http://dx.doi.org/10.1007/s10103-005-0365-7 LMSCEZ 1435-604X Google Scholar
Y. Feng et al.,
“Assessment of autofluorescence to detect the remineralization capabilities of sodium fluoride, monofluorophosphate and non-fluoride dentifrices. A single-blind cluster randomized trial,”
Caries Res., 41
(5), 358
–364
(2007). http://dx.doi.org/10.1159/000104793 CAREBK 0008-6568 Google Scholar
O. Durmusoglu, D. A. Tağtekin and F. Yanikoğlu,
“Clinical evaluation of demineralization and remineralization of intact root surface lesions in the clinic by a quantitative light-induced fluorescence system,”
Lasers Med. Sci., 27
(2), 397
–402
(2012). http://dx.doi.org/10.1007/s10103-011-0899-9 LMSCEZ 1435-604X Google Scholar
A. F. Zandoná et al.,
“Longitudinal analyses of early lesions by fluorescence: an observational study,”
J. Dent. Res., 92
(7 Suppl), 84S
–89S
(2013). http://dx.doi.org/10.1177/0022034513490167 JDREAF 0022-0345 Google Scholar
M. R. Alammari et al.,
“Quantitative light-induced fluorescence (QLF): a tool for early occlusal dental caries detection and supporting decision making in vivo,”
J. Dent., 41
(2), 127
–132
(2013). http://dx.doi.org/10.1016/j.jdent.2012.08.013 JDENAB 0300-5712 Google Scholar
K. Markowitz, R. M. Stenvall and M. Graye,
“The effect of distance and tooth structure on laser fluorescence caries detection,”
Oper. Dent., 37
(2), 150
–160
(2012). http://dx.doi.org/10.2341/10-179-L 0361-7734 Google Scholar
E. S. Ghaname et al.,
“Correlation between laser fluorescence readings and volume of tooth preparation in incipient occlusal caries in vitro,”
J. Esthet. Restor. Dent., 22
(1), 31
–39
(2010). http://dx.doi.org/10.1111/jerd.2010.22.issue-1 1496-4155 Google Scholar
O. H. Tung et al.,
“Characteristics of subgingival calculus detection by multiphoton fluorescence microscopy,”
J. Biomed. Opt., 16
(6), 066017
(2011). http://dx.doi.org/10.1117/1.3593150 JBOPFO 1083-3668 Google Scholar
F. Krause, A. Braun and M. Frentzen,
“The possibility of detecting subgingival calculus by laser-fluorescence in vitro,”
Lasers Med. Sci., 18
(1), 32
–35
(2003). http://dx.doi.org/10.1007/s10103-002-0241-7 LMSCEZ 1435-604X Google Scholar
W. Buchalla, A. M. Lennon and T. Attin,
“Fluorescence spectroscopy of dental calculus,”
J. Periodontal Res., 39
(5), 327
–332
(2004). http://dx.doi.org/10.1111/j.1600-0765.2004.00747.x JPDRAY 0022-3484 Google Scholar
E. Kurihara,
“Detection of subgingival calculus and dentine caries by laser fluorescence,”
J. Periodontal Res., 39
(1), 59
–65
(2004). http://dx.doi.org/10.1111/j.1600-0765.2004.00712.x JPDRAY 0022-3484 Google Scholar
M. Folwaczny et al.,
“Subgingival calculus detection with fluorescence induced by 655 nm InGaAsP diode laser radiation,”
J. Periodontol., 73
(6), 597
–601
(2002). http://dx.doi.org/10.1902/jop.2002.73.6.597 JOPRAJ 0022-3492 Google Scholar
F. Shakibaie and L. J. Walsh,
“Surface area and volume determination of subgingival calculus using laser fluorescence,”
Lasers Med. Sci., 29
(2), 519
–524
(2014). http://dx.doi.org/10.1007/s10103-012-1242-9 LMSCEZ 1435-604X Google Scholar
O. H. Tung et al.,
“Detection of subgingival calculus through oral gum in vitro using two-photon fluorescence microscopy,”
Conf. Proc. IEEE Eng. Med. Biol. Soc., 2008 4051
–4054
(2008). Google Scholar
Z. Badran et al.,
“Laser-induced fluorescence for subgingival calculus detection: scientific rational and clinical application in periodontology,”
Photomed. Laser Surg., 29
(9), 593
–596
(2011). http://dx.doi.org/10.1089/pho.2010.2951 PLDHA8 1549-5418 Google Scholar
F. Krause et al.,
“Evaluation of selective calculus removal by a fluorescence feedback-controlled Er:YAG laser in vitro,”
J. Clin. Periodontol., 34
(1), 66
–71
(2007). http://dx.doi.org/10.1111/cpe.2007.34.issue-1 JCPEDZ 0303-6979 Google Scholar
F. Krause et al.,
“Detection of subgingival calculus with a novel LED-based optical probe,”
J. Periodontol., 76
(7), 1202
–1206
(2005). http://dx.doi.org/10.1902/jop.2005.76.7.1202 JOPRAJ 0022-3492 Google Scholar
Q. Li et al.,
“Review of spectral imaging technology in biomedical engineering: achievements and challenges,”
J. Biomed. Opt., 18
(10), 100901
(2013). http://dx.doi.org/10.1117/1.JBO.18.10.100901 JBOPFO 1083-3668 Google Scholar
G. Lu and B. Fei,
“Medical hyperspectral imaging: a review,”
J. Biomed. Opt., 19
(1), 010901
(2014). http://dx.doi.org/10.1117/1.JBO.19.1.010901 JBOPFO 1083-3668 Google Scholar
Biography |