|
|
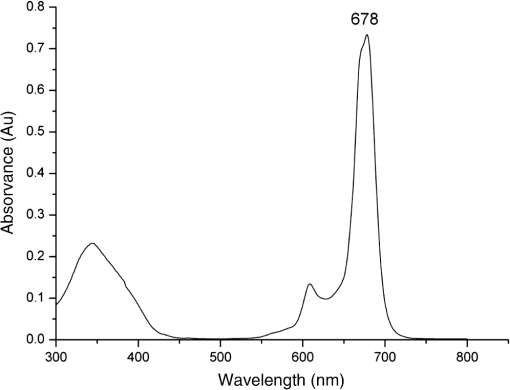
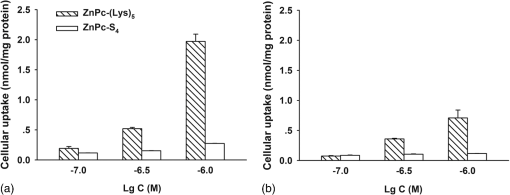
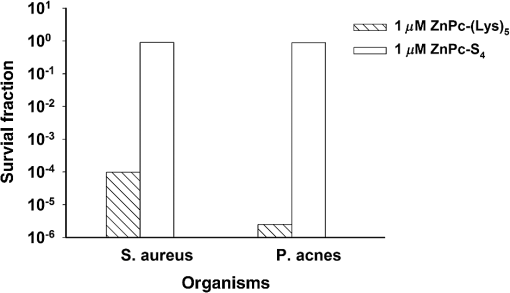
1.IntroductionThe most common bacterial infections, such as cellulitis, abscesses, and postsurgical infections, are usually caused by pathogens like Staphylococcus aureus1 and Propionibacterium acnes2 that may lead to serious local and systemic complications.3 For example, S. aureus can cause a range of illnesses, from minor skin infections to life-threatening diseases such as pneumonia, meningitis, osteomyelitis, endocarditis, toxic shock syndrome, bacteremia, and sepsis.4 In the past 60 years, antibiotics have been critical in the fight against infectious disease caused by these bacteria and other microbes. However, the broad application of antibiotics leads to bacterial resistance and becomes an increasing public health problem. Nowadays, about 70% of the bacteria that cause infections in hospitals are resistant to at least one of the drugs most commonly used for treatment. The threat of bacterium S. aureus is not only due to its distribution and pathogenicity but also to its ability to overcome antimicrobial agents.5 Antimicrobial peptides, also called host defense peptides, are an important component of the natural defenses of most living organisms against invading pathogens and have become an important research direction in the past two decades.6,7 The discovery of natural antibacterial peptides, including histatins, defensins, cathelicidins, magainins, cecropins, and tachyplasins, has provided a new way to fight antibiotic-resistant microorganisms. The wide spectrum of antimicrobial activities reported for these molecules suggests that they could be used in the treatment of viral or parasitic infections. However, there are many general obstacles to move antimicrobial peptides to clinical applications,8 including the toxicity against eukaryotic cells, the stability of the peptides in vivo, the potential for cross-resistance, and the high cost of production. Photodynamic antimicrobial chemotherapy (PACT) is a new method for killing bacterial cells.9 PACT treatment utilizes visible or near-infrared light at the appropriate wavelength to excite the nontoxic photosensitizer. The excited photosensitizer undergoes intersystem crossing to long-lived triplet states and, in the presence of oxygen, transfers its energy to molecular oxygen and generates reactive oxygen species such as singlet oxygen and hydroxyl radical, which are responsible for the killing of microbial cells nearby. One of the advantages of PACT in the inactivation of microorganisms is that both antibiotic-sensitive and -resistant strains can be successfully photoinactivated. The other advantage is that repeated photosensitization of bacterial cells does not induce a selection of resistant strains.10 Although PACT is gaining increasing acceptance for the treatment of locally occurring infections such as psoriasis11 and scleroderma12 in dermatology, it is not, at present, a mainstream therapeutic option. As a key component of PACT, an ideal photosensitizer should have high absorption coefficients in the near-infrared region, where light has deep penetration into tissues, and high photostability to minimize photobleaching. Phthalocyanines, a versatile class of macrocyclic compounds featured with a high fluorescence quantum yield, long triplet lifetimes, and high triplet quantum yields, are gathering growing interest as effective photosensitizers in targeted photodynamic therapy and imaging of tumors due to their longer wavelength band absorption ( 600 to 700 nm) and higher extinction coefficients (). Selectivity to target cells rather than host mammalian cells is another key property for the photosensitizer. In addition, photosensitizers with positive charges tend to bind to cells that carry negative charges on their surfaces. Conjugation of antimicrobial peptides to phthalocynine photosensitizer is one strategy to develop antimicrobial therapy. , a phthalocyanine derivative with five positive charges, prepared as a high purity single isomer, was previously reported13 as an effective photosensitizer with high activity in both cultured tumor cells and experimental animal tumors.14 To further investigate the photodynamic inactivation of on microorganisms involved in skin bacterial infections, we evaluated the antibacterial efficacy of in vitro and in vivo using the key pathogenic factors P. acnes and S. aureus. This study may provide a safe and effective approach for the treatment of bacterial skin infections. 2.Experimental Techniques2.1.Preparation of PhotosensitizersAccording to our early published protocols,14,15 the unsymmetrical was prepared via the activation of the carboxylic acid group on ZnPc-COOH by 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide and N-hydroxysuccinimide, and a coupling to pentalysine. The synthesized was characterized by NMR [AV-400, Bruker, 400 MHz, in dimethyl sulphoxide (DMSO)], NMR (75 MHz, in DMSO), FTIR (Magna-IR 750, Nicolett), and high-resolution mass spectra–electrospray ionization (DECAX-30000 LCQ Deca XP mass spectrometer). The UV–vis absorption spectrum of in dimethylfomamide was recorded from 300 to 800 nm using quartz cuvettes with 1-cm path length on a Lambda-35 UV/vis spectrometer (PerkinElmer, Massachusetts) in DMSO. Analytical high-performance liquid chromatography (HPLC) was carried out on a C-18 reversed-phase HPLC system (Dalian Elite Analytical Instruments Co., Ltd., Dalian, China; Column: SinoChrom ODS-BP , ), using a linear gradient from 50% to 100% (v/v) of methanol:acetonitrile () at a flow rate of . The UV–vis absorption spectrum of photosensitizer in DMSO (Fig. 1) was typical of ZnPc with the strongest absorption at 678 nm (extinction coefficient of ). Furthermore, singlet oxygen () is believed to be the major cytotoxic agent involved in photodynamic therapy. The quantum yield of singlet oxygen generation of was measured in reference to ZnPc, which has a quantum yield of 0.67 in DMSO.16 Zinc phthalocyanine tetrasulfonate () with an absorption peak at 680 nm was kindly provided by Professor Naisheng Chen of Fuzhou University, China. 2.2.Microorganism and Culture ConditionAs the standard bacteria used in antibacterial activity tests according to the National Standard of the People’s Republic of China in detection and control of pathogens (GB4789.28-2013), P. acnes (ATCC 6919) and S. aureus subsp. aureus (ATCC 6538) were purchased from Beijing Zhongyuan Ltd. S. aureus were cultured in nutrient agars, and P. acnes were cultured in thioglycollate medium in anaerobic bags. Thioglycollate medium is a semisolid nutrient medium containing a low concentration of agar to prevent convection of oxygen from the surface. The thioglycollate medium was boiled before use in order to drive off the oxygen and inoculated without excessive shaking of the medium after cooling. A luminescent strain of S. aureus Xen29 (NCTC8532), a derivative of the biofilm forming S. aureus 12600 that possesses a stable copy of the modified Photorhabdus luminescens luxABCDE operon at a single integration site on the bacterial chromosome, was purchased from Caliper Life Sciences, Inc., and grown at 37°C using Luria–Bertani broth containing kanamycin ( to select for resistance encoded by the plasmid) to an absorbance of 0.5 at 600 nm corresponding to . 2.3.Cellular Uptake of Photosensitizer by BacteriaAliquots of microorganism suspension [ colony forming unit (CFU)/ml] were incubated in 96-multiwell plates (Falcon) with photosensitizer at different concentrations (, , and ) for 1 h at 37°C. The exponentially growing cells were then washed with sterile phosphate buffer saline (PBS) before lysis with NaOH [0.1 N, 1.0 ml with 1% sodium dodecyl sulfate (SDS)] to give a homogeneous solution. The fluorescence of the cell extract was measured on a microplate reader (Synergy 4, BioTek Instruments). The concentration of cellular protein was determined using a bicinchoninic acid protein assay kit (Pierce, Thermo Fisher Scientific). Standard curves were made with cell lysates treated as above with known added amounts of bovine serum albumin. Results are expressed as nmol of phthalocyanine per mg cell protein. 2.4.Antimicrobial Studies in Cultured BacteriaBacteria suspensions () were incubated in the dark at room temperature for 1 h with (at concentrations of , , , , and ) followed by the light exposure using a light-emitting diode (LED) light source (SunDynamic, Inc., Qingdao) of 680 nm and with a power of 100 mW for 1 or 2 min (i.e., light dosages at 3 or ). After illumination of the appropriate wells, cell viability was determined by incubating agar plates overnight after applying 0.1 ml from one of the tubes in a bacterial dilution series. The percentage of cell survival was determined by comparing the colony counts from treated plates to the colony counts from control plates that were incubated without the conjugate and were kept in dark for periods equal to irradiation times. 2.5.Antimicrobial Studies in Experimental AnimalsSprague–Dawley rats (purchased from Shanghai SLAC Laboratory Animal Co. Ltd., Shanghai, China) were maintained and handled in accordance with the recommendations of an Institutional Animal Care and Use Committee (IACUC). The animals were allowed free access to water throughout the course of the experiments. The experimental procedures on rats were in accordance with PerkinElmer IACUC guidelines and approved veterinarian requirements for animal care and use. Rats () weighing were anesthetized with an intraperitoneal injection of pentobarbital (, i.p.) before they were shaved on the back and treated with depilatory cream. Two excisional wounds were then made along the dorsal surface, using surgical scissors, by carefully opening the epidermal layer of the skin with one side connected. Each wound measured with at least 5 mm of unbroken skin between wounds. The bottom of the wound was panniculus carnosus, with no visible bleeding. Localized infection on the wounds was induced according to our previously published protocol13 with slight changes by inoculating a suspension () of midlog phase bioluminescent Xen29 S. aureus ( in PBS) into each wound of the rats. The bacteria was allowed to attach to the tissue for 30 min, then of (1 mM in PBS) or (1 mM in PBS) was added into the wounds. After a further 30 min were given to allow the conjugates to bind to and penetrate the bacteria under subdued room lighting, eight rats were illuminated using a 680-nm light source (SunDynamic, Inc., Qingdao) with an irradiance of 100 mW for , giving a total light fluence of for each wound. The other eight rats were kept in their cages in the dark during the whole experimental period. To measure the bacteria load after PACT treatment, we cut out the epidermis layer of the skin from rats under anesthesia. After being shredded into small pieces, the tissues were mixed with PBS, and the bioluminescence signals were measured on a Synergy™ 4 multimode microplate reader (BioTek Instruments, Winooski, Vermont). The viability of bacteria after PACT treatment was measured by comparing the luminescence signal to that of a control group treated with saline. All rats were kept in cages after the treatment. Their wound areas were measured in two dimensions each day for 12 days. To precisely observe the early wound healing after different treatments, the laser speckle contrast imaging (LSCI) system (MoorFLPI-2, Moor Instruments Ltd., United Kingdom) was used to monitor cutaneous blood flow in the wound area after PACT treatment ( weeks later). The spatiotemporal characteristics of blood flow under the wound area were addressed. 3.Results and Discussion3.1.Preparation of Photosensitizer ZnPc-(Lys)5The structure of was confirmed by NMR spectroscopy and mass spectrometry as described previously.13–15 Furthermore, the quantum yield for singlet oxygen photogeneration for in DMSO was determined to be , which is similar to that for ZnPc (0.67),16 showing that the coupling of a positively charged pentalysine group does not significantly alter the generation of singlet oxygen. 3.2.Cellular Uptake of Photosensitizer by BacteriaThe uptake profile of a photosensitizer is important in the clinical setting in order to adjust the dose for effective treatment.17 It is believed that bacteria P. acnes and S. aureus are the main pathogenic factors involved in some skin infections, like cellulitis, abscesses, and postsurgical infections. In the current study, we measured the uptake of photosensitizer in the above-mentioned bacteria. Meanwhile, the negatively charged ZnPc compound, , was used as a control. The uptake of was shown in a dose-dependent manner with higher concentration of ZnPc leading to higher cellular uptake on both bacteria we measured (Fig. 2). Compared with the anionic photosensitizer , exhibited much higher cellular uptake amounts in both bacteria (S. aureus and P. acnes). This enhanced uptake amount of is likely due to the binding of the positively charged to the outer membrane of bacteria that bears a strong negative charge.18 Furthermore, we noticed that the uptake amount of (at ) in S. aureus ( protein) was about 2.7 times more than that in P. acnes ( protein). 3.3.Antimicrobial Studies in Cultured BacteriaWith increasing numbers of small, naturally occurring antibacterial peptides being discovered, the mechanism of action of these peptides is being intensively investigated.19–21 A common factor in all the structures is the polycationic charge due to lysine, histidine, and arginine residues in the amino acid sequence, and the polycationic charge is probably responsible for their initial binding to bacteria. In this study, we conjugated a pentalysine moiety to ZnPc to selectively target bacteria for photodestruction and tested the antibacterial activities of under two different light dosages (3 and ) against S. aureus. Figure 3 shows the antibacterial activities of [Fig. 3(a)] and [Fig. 3(b)] against S. aureus at different light dosages (3 and , respectively). It is obvious that inhibited the bacterial growth in light dosage-dependent and photosensitizer dose-dependent manners [Fig. 3(a)]. In contrast, did not show significant toxicity to S. aureus under the same conditions with the same light and photosensitizer dosages [Fig. 3(b)]. The pronounced photodynamic effect of the cationic on S. aureus may be due to the electrostatic attraction between the photosensitizer and the negatively charged membrane of the bacterium. Fig. 3(a) Dose-dependent antimicrobial effects of and (b) on S. aureus under two different light doses (3 and , respectively).  Moreover, did not show significant toxicity to the bacterium in the absence of light illumination (data not shown), suggesting a broad safety margin of with concentration followed by a light dosage at . We further investigated the antimicrobial activities of against P. acnes, the primary pathogen responsible for cystic acne, under a light dose at using a colony-counting method. It showed that irradiation of P. acnes cells treated with (at a concentration of ) caused a 5 to 6 log reduction of the CFU (Fig. 4). In comparison, the survival fraction of P. acne was about only 4 log reduction of the CFU, which was much smaller than that of S. aureus. This result was in line with the different amount of cellular uptakes we observed (Fig. 2). 3.4.Antimicrobial Studies in Experimental AnimalsThe method using genetically engineered bacteria that emit luminescence to monitor bacterial numbers and viability in real time in living animals so far has been demonstrated in several models.22,23 In the current studies, we evaluated the in vivo efficacy of on skin disorder-related bacteria using a localized infection animal model by inoculating the luminescent strain of S. aureus (Xen29) into excisional wounds on the back of rats. We estimated that the luminescence signal was linearly proportional to live bacterial CFU in the range of to CFU. In our experiments, about 2 million CFU of the luminescent S. aureus from a midlog culture in were applied onto each wound () made on the back of anesthetized rats. The antibacterial efficacy of on skin disorder-related bacteria was evaluated by measuring the bacterial load right after the PACT treatment and monitoring the wound size for 12 days after the PACT treatment in order to detect the wound healing rate. We observed that dramatically reduced the bacterial load in the wounds upon light irradiation (680 nm, ), whereas without light irradiation or with the anionic photosensitizer (in the presence or absence of light irradiation) did not show an antibacterial effect upon the excisional wounds on the back of rats (Fig. 5). These results show that the cationic has a strong antimicrobial effect in animal models and is more effective than anionic photosensitizer . Fig. 5Reduction of viable luminescent S. aureus strain (Xen29) in infected incision wounds on rats upon incubation with () and light exposure (680 nm, ). Data points are means of values from wounds on rats, and bars are standard error of the mean (SEM). 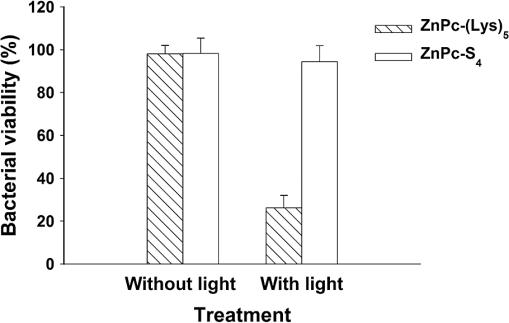 In the presence of light, dramatically promoted wound healing in rats from the second day after the treatment compared with (Fig. 6). This accelerating effect on wound healing is much stronger in the presence of light (680 nm, ) compared to the case without the irradiation. Such wound-healing promotional activities were previously reported with two different photosensitizers (5-aminolevulinic acid at and hematoporphyrin derivative at ) in an open excision wound model with rats.24 Interestingly, two other reports25,26 showed that PACT treatment did not have any effect on wound healing. The reason for these conflicting results is not yet clear; it could probably be explained by the use of different photosensitizers and requires further study. Fig. 6Effects of () on wound recovery of S. aureus infected excisional wounds with rats in the presence or absence of light irradiation (680 nm, ). Each wound was infected with CFU S. aureus 30 min before the photodynamic treatment with photosensitizers. Wounds were measured in two dimensions every day after the infection, and the areas were calculated. Data points are means of values from the corresponding wound on rats and bars are SEM. 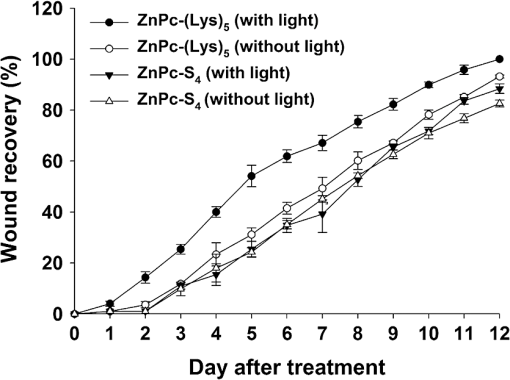 We noticed that the wound recovery rate was significantly enhanced from the second day to the fifth day after PACT with (Fig. 6) and slowed down afterward. This observation is possibly due to the metabolism of and suggests that PACT with applied repeatedly for a certain interval of time () would promote the recovery of infected incision wounds on rats. To further evaluate the wound healing process in bacterial skin infections with PACT treatment, we imaged the blood flow under the wound area upon all wounds healing (2 weeks later) using an LSCI system, which has been used widely to image cutaneous blood flow.27,28 We observed that PACT with in the presence of light irradiation (680 nm, ) significantly reduced the blood flow under the wound area (-fold blood flow as normal skin, Fig. 7(B-c), whereas PACT with showed -fold blood flow as normal skin in the presence or absence of light irradiation [Fig. 7(B-a)]. These results demonstrated that PACT with significantly relieved the symptoms of inflammation during the wound healing process [Fig. 7(C)]. Furthermore, we observed that PACT with in the absence of light irradiation partially reduced the blood flow under the wound area [-fold blood flow under normal skin, Fig. 7(B-b)], indicating that ambient light illumination alone was helpful in promoting the wound healing process under PACT with . Fig. 7In vivo speckle imaging of S. aureus infected excisional wounds with rats treated with or . (A) Schematic diagram of the laser speckle imaging system. (B) Three representative speckle images of the wound-skin rats treated with ZnPc-S4 (a) or with (c) or without (b) irradiation (680 nm, ). (C) Analysis of the blood flow ratio under wound-skin of rats 2 weeks after PACT with or . 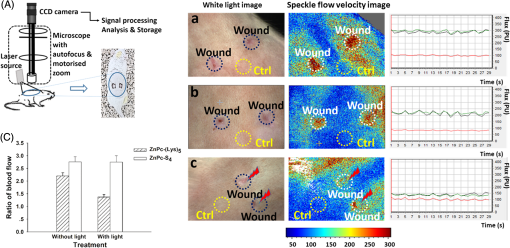 The LSCI system used in the current study allows for real-time monitoring of the skin microvascular structural and functional information. It shows great potential for monitoring blood flow, but the spatial resolution suffers from the scattering of tissue.28,29 A combination method of LSCI and skin optical clearing is now attracting increasing attention.28,30,31 The physiological effect of the optical-clearing agents on skin, such as inflammation, seems limited but requires further evaluation.32 Typically, PACT treatment uses laser light sources. For example, a recent report showed the effectiveness of laser therapy with a wavelength of 850 nm in the prevention of caries and gingivitis in adolescents.33 We used LED light sources with a power of 100 mW in this study and found it strong enough to produce significant antimicrobial photodynamic effects, in combination with our cationic photosensitizer . The use of battery-powered, inexpensive, and portable LED light sources may make possible a low-cost and efficient deployment of systems to be used for wound decontamination. 4.ConclusionsWith the widespread occurrence of antibiotic resistance among pathogenic bacteria, additional methods of killing bacteria in wounds are being sought vigorously. We herein report the use of a zinc phthalocyanine derivative, pentalysine -carbonylphthalocyanine zinc ), in PACT, the promising antimicrobial effects on bacterial infected skin, and the increased rate of healing after PACT treatment in an animal model. In conclusion, our study demonstrated that phthalocyanine-based photosensitizer shows a specific affinity for bacterial cells. Compared with , showed more efficient uptake by bacterial cells and enhanced antimicrobial effects in vitro, as well as a significantly increased healing rate of S. aureus infected excisional wounds on rats. Overall, is a promising antimicrobial photosensitizer for the safe and effective treatment of bacterial skin infection. AcknowledgmentsThis work was financially supported by the National Natural Science Foundation (81171634) and the Fujian Natural Science Foundation (2013J01387 and 2013J01066). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the article. ReferencesP. Francois et al.,
“Proteomic approaches to study Staphylococcus aureus pathogenesis,”
J. Proteomics, 73 701
–708
(2010). http://dx.doi.org/10.1016/j.jprot.2009.10.007 Google Scholar
A. M. Layton,
“Optimal management of acne to prevent scarring and psychological sequelae,”
Am. J. Clin. Dermatol., 2 135
–141
(2001). http://dx.doi.org/10.2165/00128071-200102030-00002 Google Scholar
R. L. Nichols and S. Florman,
“Clinical presentations of soft-tissue infections and surgical site infections,”
Clin. Infect. Dis., 33
(Suppl. 2), S84
–S93
(2001). http://dx.doi.org/10.1086/321862 Google Scholar
L. Baba-Moussa et al.,
“Virulence factors produced by strains of Staphylococcus aureus isolated from urinary tract infections,”
J. Hosp. Infect., 68 32
–38
(2008). http://dx.doi.org/10.1016/j.jhin.2007.10.010 Google Scholar
N. Cimolai,
“MRSA and the environment: implications for comprehensive control measures,”
Eur. J. Clin. Microbiol. Infect. Dis., 27 481
–493
(2008). http://dx.doi.org/10.1007/s10096-008-0471-0 CECED9 Google Scholar
A. Peschel,
“How do bacteria resist human antimicrobial peptides?,”
Trends Microbiol., 10 179
–186
(2002). http://dx.doi.org/10.1016/S0966-842X(02)02333-8 Google Scholar
E. Guani-Guerra et al.,
“Antimicrobial peptides: general overview and clinical implications in human health and disease,”
Clin. Immunol., 135 1
–11
(2010). http://dx.doi.org/10.1016/j.clim.2009.12.004 Google Scholar
Jr. R. C. Moellering,
“Discovering new antimicrobial agents,”
Int. J. Antimicrob. Agents, 37 2
–9
(2011). http://dx.doi.org/10.1016/j.ijantimicag.2010.08.018 Google Scholar
G. P. Tegos et al.,
“Inhibitors of bacterial multidrug efflux pumps potentiate antimicrobial photoinactivation,”
Antimicrob. Agents Chemother., 52 3202
–3209
(2008). http://dx.doi.org/10.1128/AAC.00006-08 Google Scholar
M. Wainwright et al.,
“Photobactericidal activity of phenothiazinium dyes against methicillin-resistant strains of Staphylococcus aureus,”
FEMS Microbiol. Lett., 160 177
–181
(1998). http://dx.doi.org/10.1111/j.1574-6968.1998.tb12908.x Google Scholar
J. Dominic et al.,
“Improved response of plaque psoriasis after multiple treatments with topical 5-aminolaevulinic acid photodynamic therapy,”
Acta Derm. Venereol., 79 451
–455
(1999). http://dx.doi.org/10.1080/000155599750009898 Google Scholar
S. Karrer et al.,
“Topical photodynamic therapy for localized scleroderma,”
Acta Derm. Venereol., 80 26
–27
(2000). http://dx.doi.org/10.1080/000155500750012469 Google Scholar
Z. Chen et al.,
“An effective zinc phthalocyanine derivative for photodynamic antimicrobial chemotherapy,”
J. Lumin., 152 103
–107
(2014). http://dx.doi.org/10.1016/j.jlumin.2013.10.067 Google Scholar
Z. Chen et al.,
“Pentalysine beta-carbonylphthalocyanine zinc: an effective tumor-targeting photosensitizer for photodynamic therapy,”
ChemMedChem, 5 890
–898
(2010). http://dx.doi.org/10.1002/cmdc.201000042 Google Scholar
J. Chen et al.,
“Derivatizable phthalocyanine with single carboxyl group: synthesis and purification,”
Inorg. Chem. Commun., 9 313
–315
(2006). http://dx.doi.org/10.1016/j.inoche.2005.12.002 1387-7003 Google Scholar
N. A. Kuznetsova et al.,
“Relationship between the photochemical properties and structure of pophyrins and related compounds,”
Russ. J. Gen. Chem., 70 133
–140
(2000). Google Scholar
Z. Huang et al.,
“Photodynamic therapy of cancer—challenges of multidrug resistance,”
J. Innovative Opt. Health Sci., 08 1530002
(2015). http://dx.doi.org/10.1142/S1793545815300025 Google Scholar
G. J. Tortora, B. R. Funke and C. L. Case, Microbiology: An Introduction, The Benjamin/Cummings Publishing Company, Inc., Redwood City, California
(1992). Google Scholar
S. A. Baltzer and M. H. Brown,
“Antimicrobial peptides: promising alternatives to conventional antibiotics,”
J. Mol. Microbiol. Biotechnol., 20 228
–235
(2011). http://dx.doi.org/10.1159/000331009 JMMBFF 1464-1801 Google Scholar
F. Costa et al.,
“Covalent immobilization of antimicrobial peptides (AMPs) onto biomaterial surfaces,”
Acta Biomater., 7 1431
–1440
(2011). http://dx.doi.org/10.1016/j.actbio.2010.11.005 Google Scholar
N. K. Brogden and K. A. Brogden,
“Will new generations of modified antimicrobial peptides improve their potential as pharmaceuticals?,”
Int. J. Antimicrob. Agents, 38 217
–225
(2011). http://dx.doi.org/10.1016/j.ijantimicag.2011.05.004 Google Scholar
H. L. Rocchetta et al.,
“Validation of a noninvasive, real-time imaging technology using bioluminescent Escherichia coli in the neutropenic mouse thigh model of infection,”
Antimicrob. Agents Chemother., 45 129
–137
(2001). http://dx.doi.org/10.1128/AAC.45.1.129-137.2001 Google Scholar
T. Dai et al.,
“Photodynamic therapy for methicillin-resistant Staphylococcus aureus infection in a mouse skin abrasion model,”
Lasers Surg. Med., 42 38
–44
(2010). http://dx.doi.org/10.1002/lsm.20887 Google Scholar
R. S. Jayasree et al.,
“The influence of photodynamic therapy on the wound healing process in rats,”
J. Biomater. Appl., 15 176
–186
(2001). http://dx.doi.org/10.1106/9335-Q0NC-5XCQ-KBYK JBAPEL 0885-3282 Google Scholar
M. R. Hamblin et al.,
“Rapid control of wound infections by targeted photodynamic therapy monitored by in vivo bioluminescence imaging,”
Photochem. Photobiol., 75 51
–57
(2002). http://dx.doi.org/10.1562/0031-8655(2002)075<0051:RCOWIB>2.0.CO;2 Google Scholar
S. G. Parekh et al.,
“Photodynamic modulation of wound healing with BPD-MA and CASP,”
Lasers Surg. Med., 24 375
–381
(1999). http://dx.doi.org/10.1002/(SICI)1096-9101(1999)24:5<375::AID-LSM8>3.0.CO;2-B Google Scholar
D. Zhu et al.,
“Imaging dermal blood flow through the intact rat skin with an optical clearing method,”
J. Biomed. Opt., 15 026008
(2010). http://dx.doi.org/10.1117/1.3369739 JBOPFO 1083-3668 Google Scholar
R. Shi et al.,
“Accessing to arteriovenous blood flow dynamics response using combined laser speckle contrast imaging and skin optical clearing,”
Biomed. Opt. Express, 6 1977
–1989
(2015). http://dx.doi.org/10.1364/BOE.6.001977 BOEICL 2156-7085 Google Scholar
D. Briers et al.,
“Laser speckle contrast imaging: theoretical and practical limitations,”
J. Biomed. Opt., 18 066018
(2013). http://dx.doi.org/10.1117/1.JBO.18.6.066018 JBOPFO 1083-3668 Google Scholar
Y. Ding et al.,
“Signal and depth enhancement for in vivo flow cytometer measurement of ear skin by optical clearing agents,”
Biomed. Opt. Express, 4 2518
–2526
(2013). http://dx.doi.org/10.1364/BOE.4.002518 BOEICL 2156-7085 Google Scholar
J. Wang, R. Shi and D. Zhu,
“Switchable skin window induced by optical clearing method for dermal blood flow imaging,”
J. Biomed. Opt., 18 061209
(2013). http://dx.doi.org/10.1117/1.JBO.18.6.061209 JBOPFO 1083-3668 Google Scholar
D. Zhu et al.,
“Recent progress in tissue optical clearing,”
Laser Photonics Rev., 7 732
–757
(2013). http://dx.doi.org/10.1002/lpor.201200056 LPRAB8 1863-8880 Google Scholar
D. Y. Suetenkov, A. P. Petrova and T. L. Kharitonova,
“Photo activated disinfection efficiency of low-intensity laser and comprehensive prevention of caries and gingivitis in adolescents using bracket system,”
J. Innovative Opt. Health Sci., 08 1541002
(2015). http://dx.doi.org/10.1142/S1793545815410023 Google Scholar
BiographyZhuo Chen is a full professor at the Fujian Institute of Research on the Structure of Matter (FJIRSM), Chinese Academy of Sciences. She received her PhD in biochemistry and molecular biology from FJIRSM following her MD degree from Fujian Medical University and her BS degree from Chinese Pharmaceutical University. Her current research interests focus on design and synthesis of photosensitizers and the evaluation of their pharmacological effects through experiments in cells and animals. She is a member of SPIE. |