|
|
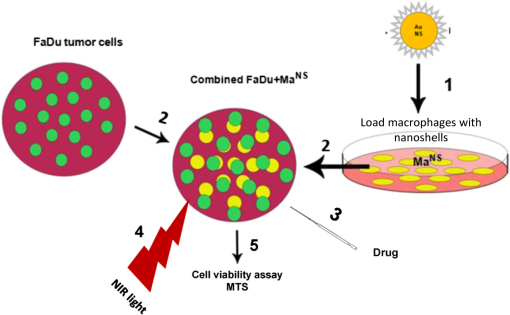
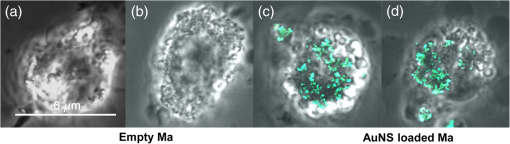
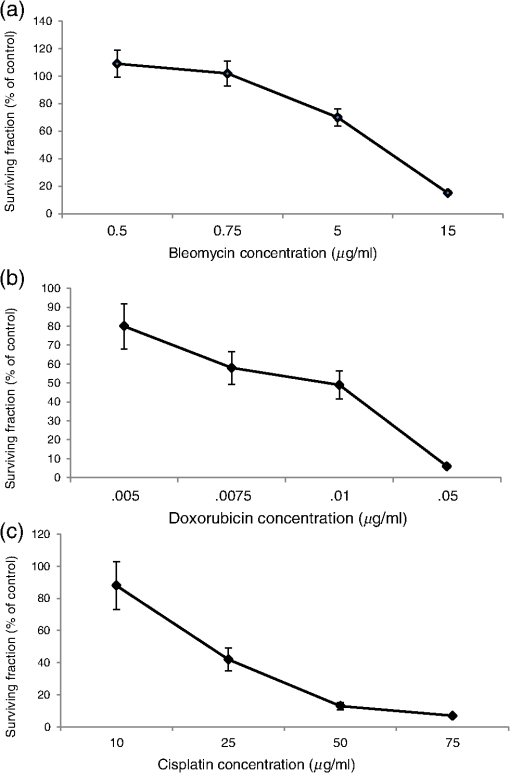
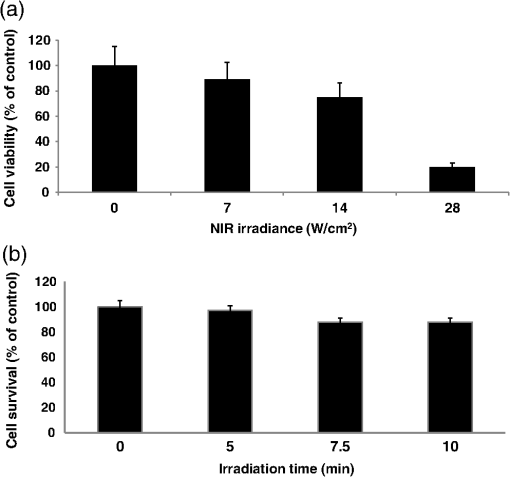
1.IntroductionHead and neck squamous cell carcinoma (HNSCC) is the most common type of malignant tumor in the upper aerodigestive tract. Standard therapy for HNSCC is surgical resection followed by a combination of radiation and chemotherapy to eliminate remaining tumor cells or metastases. Despite advancements in imaging and surgical techniques to achieve organ preservation, there has been little improvement in survival rates over the past 50 years.1 In order to improve the effects of conventional therapies, MHT has been combined with chemotherapy or ionizing radiation in the treatment of a variety of HNSCC as adjuvant therapy.2–7 MHT itself does not appear to induce chromosomal DNA strand breaks directly, but can alter chromatin structure influencing DNA repair.8 In contrast, heat treatment at temperatures over 46 to 50°C induces both apoptosis and necrosis with the type of death changing from apoptosis to necrosis above a certain threshold temperature. Furthermore, tumor permeability to macromolecules, such as chemotherapeutic agents, increases in the presence of heating, thus providing the rationale for combination therapies consisting of MHT and chemotherapy. The majority of studies on MHT-enhanced chemotherapies have been conducted with systemic heating, but recently, the combination of chemotherapy with the use of NIR light and photoactivable nanoparticles, such as gold nanospheres or nanorods, to induce MHT, has attracted attention.9–12 Gold nanoshells (AuNS) are a new class of optically tunable nanoparticles composed of a dielectric silica core coated with a thin layer of gold.13 By adjusting the thickness of the core and shell, AuNS can be manipulated to absorb and scatter light at specific wavelengths ranging from the visible to NIR. When AuNS are exposed to light, the electric field induces collective oscillation of the conduction-band electrons on the surface of the particle—the so-called surface plasmon resonance effect.14 De-excitation results in the generation of heat. AuNS are highly efficient photothermal agents due to their strong absorption cross-section and excellent optical-to-thermal energy conversion efficiency. Previous studies of the effects of MHT on drug efficacy have combined heat converting agents such as photothermal dyes or nanoparticles, directly incorporated within the tumor cells themselves, and hyperthermia induced by laser activation.9–12 This approach is, however, difficult to facilitate in vivo due to the inefficient transport of photothermal nanoparticles into tumors.15,16 An alternative to direct injection of nanoparticles is the use of certain types of cells, which are known to track tumors, as transport delivery vectors.17,18 In particular, macrophages (Ma) are well suited as transport vehicles for nanoparticles since they can be patient derived and can carry large payloads. Several studies in experimental animal models have demonstrated that exogenous intravenously injected loaded Ma can be detected in implanted tumors.19–22 Furthermore, previous in vitro studies have demonstrated that Ma can internalize a sufficient number of AuNS for efficient photothermal therapy (PTT) in models consisting of tumor cell and Ma monolayers or three-dimensional multicellular hybrid spheroids.23–26 In these studies, high levels of NIR exposure were necessary, even under ideal in vitro conditions, to raise tumor cell temperatures to toxic levels (50°C). These high energy levels can be difficult to achieve in vivo for deep-seated pathologies.27 Here we report the results of in vitro experiments that demonstrate an increased efficacy of commonly used chemotherapeutic agents in response to MHT induced by NIR activation of AuNS-loaded Ma. A synergistic effect between these two modalities allows much lower NIR energies to be employed for an equivalent toxic effect compared to PTT. The model system consisted of monolayers of AuNS-loaded murine Ma () in coculture with HNSCC tumor target cells. Treatment efficacy was determined by comparing cytotoxicity of the combined treatment to that of each individual treatment, chemotherapy or PTT. Since the primary goal of PTT is to damage cells directly by inducing temperatures above toxic levels (46 to 50°C), the terminology moderate photothermal therapy (MPTT) is used throughout this paper to designate MHT induced by NIR activation of . 2.Materials and Methods2.1.Cell LinesP388D1 murine lymphocytic monocytes (Ma) (ATCC# CCL-46) and human hypopharyngeal squamous carcinoma cells (FaDu) were maintained in Dulbecco’s modified Eagle’s medium (DMEM; Life Technologies Corp., Carlsbad, California) supplemented with 10% fetal bovine serum, 25 mM HEPES buffer (), of penicillin, and of streptomycin. FaDu is an adherent cell line and was maintained as a monolayer, while the Ma line was grown in suspension. Both cell lines were maintained under physiological conditions in an incubator (37°C, 5.0% , and 95% humidity). 2.2.NanoparticlesAuNS (AuroShell™) were purchased from Nanospectra Biosciences Inc. (Houston, Texas). NS were coated with polyethylene glycol (PEG) in order to prevent aggregation. AuNS were supplied as a suspension in deionized water () and consisted of a 120-nm-diameter silica core encased in a gold shell of 15 nm thickness giving a total particle diameter of 150 nm. 2.3.IncubationWe seeded P388D1 Ma in 35 mm cell culture dishes in 2 mL of culture medium. The dishes were incubated overnight to allow the cells to settle. Culture medium was exchanged for of PEGylated () AuNS colloid in 1.9 mL of culture medium. The were incubated for 24 h at 37°C and then treated with mitomycin C for 1 h to prevent cell division. After the Ma had ingested the AuNS, they no longer remained in suspension culture and strongly adhered to the plastic surface. This was in contrast to their normal suspension culturing. The were washed three times with Hanks’ balanced salt solution with calcium chloride and magnesium chloride (Gibco, Carlsbad, California) to wash away the excess of noningested NS and mitomycin C residues. were then detached with trypsin and a rubber spatula, washed, and counted. The concentration of AuNS in the Ma was studied using a UV-Vis-NIR spectrophotometer (Varian UV-Vis-NIR spectrophotometer Cary 6000i, Varian) as previously described in detail.24 Briefly, in order to calculate the % uptake of AuNS in Ma, reference solutions containing AuNS in the absence of Ma were used. Consequently, Ma incubated under similar conditions but in the absence of AuNS was similarly treated, and their absorbance value subtracted from those of the groups to give the pure absorbance of the incorporated nanoparticles. % uptake of AuNS was calculated by the absorbance of incorporated AuNS at divided by the absorption of the AuNS alone . 2.4.Two-Photon MicroscopyWe plated out empty Ma or on 35-mm glass-bottomed imaging dishes. The cells were incubated overnight in clear buffer. Two-photon micrographs were generated using an inverted Zeiss laser-scanning microscope (LSM 410, Carl Zeiss, Jena, Germany). This system allows the differential visualization of cells and nanoparticles using confocal and two-photon microscopy. The reflectance from the ingested AuNS was pseudo-colored green to allow their identification. 2.5.Cell Proliferation AssayThe CellTiter 96® AQueous One Solution Cell Proliferation Assay (MTS; Promega, Madison, Wisconsin) was used for determining the number of viable cells. Following treatment, MTS reagent () was added to each well (96-well plate) containing cells and DMEM. The plates were incubated for 1 h and transferred to an Infinite® M1000 PRO microplate reader (TECAN Group Ltd., Mannedorf, Germany) for absorbance reading at 490 nm. MTS values obtained from methanol treated cultures (100% dead) were considered background and subtracted from all experimental results. The absorption at 490 nm, due to the presence of AuNS and dead cells, was therefore compensated for. 2.6.Drug ToxicityFaDu cells and ( FaDu and ) were pipetted into the wells of a 96-well plate. A total of three well plates were prepared, one for each chemotherapeutic drug. Drugs were added to DMEM medium to obtain the following concentrations: 0.1 to of bleomycin, 0.001 to of doxorubicin, and 1 to of cisplatin. In all cases, cell suspensions and chemotherapeutic agents were incubated for five days at 37°C, after which time MTS reagent () was added to each well and the incubation continued for an additional 60 min. The MTS assay was read in a microplate reader (ELx Bio-Tek Instruments). The pharmacological potency resulting in to 90% survival was used in subsequent combined therapy studies. 2.7.Moderate Photothermal Therapy ToxicityA fiber-coupled diode laser (Intense, North Brunswick, New Jersey) was used to irradiate cells at a wavelength of 810 nm. Each well was irradiated separately using an irradiance of 7, 14, or for 7.5 min. Additionally, in order to establish the time to reach temperature equilibrium, three irradiation times were investigated (5, 7.5, and 10 min) using a laser irradiance of corresponding to radiant exposures of 2.10, 3.15, and , respectively. The radiant exposure resulting in survival was used in subsequent combined therapy studies. All irradiations were performed at a constant temperature of 37°C. After irradiation, the plates were incubated for five days. Following incubation, MTS assays were performed as previously described. The experiments were performed in triplicate. 2.8.Combined Chemotherapy and Moderate Photothermal TherapyThe setup for combined chemotherapy and NIR light treatment is shown in Fig. 1. FaDu and were combined at a ratio of of 2:1. Based on the toxicity results for each of the three drugs, concentrations resulting in 70 to 90% survival were chosen. Therefore, bleomycin, cisplatin, and doxorubicin were added to the combined FaDu cells and Ma in the 96-well plates prior to irradiation. Each photothermal-treated well was irradiated separately using an irradiance of (8 mm beam diameter) for 7.5 min resulting in a radiant exposure of . Otherwise, the irradiation protocol using the 810 nm fiber-coupled diode laser was identical to that previously described in Sec. 2.7. Following treatment, the plates were incubated for five days and MTS assays were performed. 2.9.Statistical AnalysisData analysis was performed in Microsoft Excel. All data were normalized to the control group of each individual experiment and all error bars represent standard deviations. GraphPad QuickCalcs (GraphPad Software, Inc., La Jolla, CA) was used for Student’s test; values less than 0.05 were considered significant. In order to determine the degree of interaction between MPTT and the chemo-agents, the following equation was used:28 The numerator includes the product of the surviving fraction (SF) of the individual treatments separately and the denominator includes the SF of the combined treatments. A value of indicates an additive effect, while values of or indicate antagonistic or synergistic effect, respectively. 3.Results3.1.Macrophages Endocytosis of Polyethylene Glycolylated Gold NanoshellWe incubated P388D1 cells with PEGylated AuNS for 24 h. Ma showed significant uptake of AuNS as measured by UV/Vis spectrophotometry at . The % uptake of PEGylated AuNS in the Ma was 4% corresponding to approximately . The uncertainty in AuNS concentration was due to cell division during incubation and was estimated based on the doubling time of the Ma cell line (32 h).29 Aggregates of AuNS in the cytoplasm of Ma could be visualized with two-photon microscopy for empty [Figs. 2(a) and 2(b)] and loaded [Figs. 2(c) and 2(d)] Ma. In previous reports, TEM images of revealed extensive intracellular presence of the nanoparticles, in small aggregates, inside vacuoles, which were dispersed throughout the cellular cytoplasm.23,24 3.2.Drug ToxicityThe bleomycin titration results [Fig. 3(a)] show that the is in the range of 5 to . As shown in Fig. 3(b), doxorubicin was the most potent of the three drugs tested (), while cisplatin () was the least toxic [Fig. 3(c)]. Based on the previously established criterion of 70 to 90% survival, the results in Figs. 3(a)–3(c) suggest that doxorubicin, bleomycin, and cisplatin, concentrations of 0.05, 5, and , respectively, should be used in the combined treatments. 3.3.Photothermal ToxicityThe effects of increasing NIR laser irradiance on cell viability were determined for 7, 14, and . Irradiation time was 7.5 min and the ratio was 2:1. As illustrated in Fig. 4(a), irradiance had limited effect on cell viability (89% survival) compared to nontreated controls. At irradiances of 14 or , significant MPTT toxicity was observed: 71 and 20%, respectively. The effects of MPTT treatment times at were also investigated [Fig. 3(b)]. Irradiation times of 5 min resulted in minimal cell toxicity, while 7.5 and 10 min irradiations produced 89% cell survival. The observation that there was no increase in cell lethality between 7.5 and 10 min irradiation times indicated that the cell hybrid cultures had achieved a thermal steady state. Based on these results, an irradiation time of 7.5 min and an irradiance of were chosen for the combined MPTT and chemotherapy studies. 3.4.Combined Chemotherapy and Moderate Photothermal Therapy Induced HyperthermiaIn order to investigate the degree of interaction between the chemotherapeutic agents and NIR-induced MHT, suboptimal levels of both drug concentrations and MPTT levels, as determined in the above experiments, were used. The effects on drug efficacy of Ma-mediated MPTT MHT for all three drugs are shown in Fig. 5. The cell survival values for controls (drug-only) were compared to the results obtained by MPTT-induced MHT. Student’s tests were used to verify significant differences between these values and are indicated in Fig. 5 by an asterisk (*). When cell survival was compared to drug-only controls, there was a significant decrease in cell survival for all three drugs by MPTT-induced MHT (). The corresponding alpha values, calculated from Eq. (1), are shown in Table 1 and indicate additive effects for the combined MPTT/doxorubicin and the combined MPTT/bleomycin groups, with a synergistic effect noted for the combined MPTT/cisplatin treatment. Fig. 5Combined chemotherapy and MPTT. Student’s tests were used to verify significant differences between controls and MPTT-induced MHT. Significant differences () are denoted by asterisks. The surviving fraction was normalized to the no-treatment controls. Each data point corresponds to the of three trials. 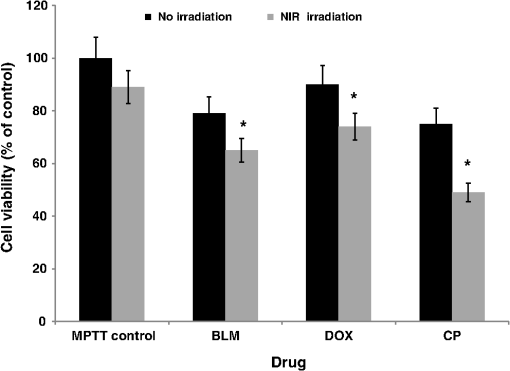 Table 1Degree of interaction between NIR-induced MHT and chemotherapy.
4.DiscussionCurrent treatment for many cancers, such as brain, hypopharyngeal squamous cell carcinomas, and breast cancers, include surgical resection followed by various treatments such as chemotherapy and/or radiotherapy. The goal of subsequent treatments is to eliminate the malignant cells residing in the margin surrounding the resection cavity, thereby reducing or eliminating recurrence. Unfortunately, in many cases, none of the standard treatment regimens have proven to be successful, suggesting that alternative therapeutic approaches are required. The results of the experiments reported here clearly indicated that a subpopulation of AuNS-loaded Ma sequestered among tumor cells, when irradiated with NIR light, significantly enhanced the efficacy of certain chemotherapeutic drugs. This enhancement was achieved at moderate levels of NIR laser powers, an observation of importance when considering eventual clinical translation. Previous in vitro and in vivo studies have combined heat converting nanoparticles directly incorporated within the tumor cells themselves.9–11,30 Although AuNS can be readily incorporated into tumor cells in vitro, this is much more difficult to achieve in vivo. Following administration in vivo, nanoparticles passively accumulate in tumors via the enhanced permeability and retention (EPR) effect by passing through fenestrations in the endothelial tumor vasculature and are retained in the tumor due to impaired lymphatic drainage. EPR is a passive effect and, as such, no active transport is involved, thus limiting the effectiveness of nanoparticle-based imaging and therapy.16,17 In contrast, since the incorporation of NS into Ma can be done ex vivo, using Ma isolated from the tumor-bearing individual, optimum conditions for their uptake can be controlled. A number of studies have demonstrated the efficacy of PTT using AuNs-loaded Ma or monocytes as NIR laser-induced hyperthermia generators in in vitro systems using human glioma spheroids and human head and neck squamous carcinoma cell lines.23–25 The results of Trinidad et al. are particularly relevant to the present work since the same cell line (FaDu) was used.31 The irradiation parameters of for 7.5 min exposures and the use of an FaDu to monocyte ratio of 2:1 in the present study were chosen based on the results of Trinidad et al. who showed that an irradiance of for 5 min (radiant exposure of ) resulted in survival in a 2:1 mixture of FaDu cells and NS-loaded Ma.31 This is in excellent agreement with the results presented in Fig. 4. These investigators also observed no cytotoxicity in empty Ma exposed to and also found that this level of radiant exposure led to significant cytotoxicity, with only a 20% survival, if the Ma contained AuNS.17 A similar finding was noted by Chhetri et al.32 who found no growth inhibition in human glioma spheroids subjected to identical radiant exposures. Collectively, these results suggest that a radiant exposure of is insufficient to produce hyperthermic effects in cells devoid of AuNS. In order to investigate the degree of interaction between the chemotherapeutic agents and MHT, suboptimal levels of both modalities were determined. The results as seen in Fig. 5 and Table 1 show that concurrent treatments of MPTT with bleomycin or doxorubicin demonstrated additive effects (), while a synergistic effect () was observed for concurrent MPTT and cisplatin. Previous studies showing additive effects for doxorubicin and synergistic effects for bleomycin and cisplatin at 43.5°C11,24,25 are in good agreement with the results shown in Table 1. The mechanism of synergism between MHT (MPTT) and drug is not known in detail, but it likely has several components. For efficient drug delivery to take place, several extra- and intracellular barriers need to be overcome. MHT most probably facilitates enhanced drug efficacy by increasing cellular uptake via endocytosis, promoting endosomal escape and release of the drug into the cytosol.33–35 In addition, all three drugs are incorporated into DNA causing damage, which often results in cell death unless the damage is repaired. Since hyperthermia inhibits DNA repair, it is postulated that the addition of heat enhances the cytotoxicity of the chemotherapeutic agents via inhibition of DNA repair.8 Although the results of the in vitro study reported here have successfully demonstrated some critical steps in -mediated MPTT leading to enhanced drug effects, translation of this modality to animal experiments is clearly required. Fundamental to the concept of using cells as delivery vehicles is the ability of the loaded cells to gain access to the tumor microenvironment in sufficient numbers for effective therapy to take place. Animal experiments are planned, using the results from the in vitro study, to determine the potential of this type of combined therapy. 5.ConclusionsThe overall objective of this work was to investigate the ability of AuNS-loaded Ma when activated by NIR light to produce sufficient MHT to increase the efficacy of chemotherapeutic drugs. Suboptimal levels of both drugs and photothermal activation were determined. The results showed that MPTT combined with cisplatin resulted in synergism while additive effects were observed for concurrent treatments of MPTT for both doxorubicin and bleomycin. AcknowledgmentsThe authors are grateful for the support from the Norwegian Radium Hospital Research Foundation. Portions of this work were made possible through access to the LAMMP Program NIBIB P41EB015890 at UCI. Steen Madsen was supported, in part, by the Tony and Renee Marlon Charitable Foundation. ReferencesJ. B. Vermorken and P. Specenier,
“Optimal treatment for recurrent/metastatic head and neck cancer,”
Ann. Oncol., 21 vii252
–vii261
(2010). http://dx.doi.org/10.1093/annonc/mdq453 Google Scholar
P. Wust et al.,
“Hyperthermia in combined treatment of cancer,”
Lancet Oncol., 3
(8), 487
–497
(2002). http://dx.doi.org/10.1016/S1470-2045(02)00818-5 LOANBN 1470-2045 Google Scholar
R. Valdagni, F. Liu and D. Kapp,
“Important prognostic factors influencing outcome of combined radiation and hyperthermia,”
Int. J. Radiat. Biol. Phys., 15 959
–972
(1988). http://dx.doi.org/10.1016/0360-3016(88)90133-2 Google Scholar
N. G. Huilgol, S. Gupta and R. Dixit,
“Chemoradiation with hyperthermia in the treatment of head and neck cancer,”
Int. J. Hyperthermia, 26
(1), 21
–25
(2010). http://dx.doi.org/10.3109/02656730903418283 IJHYEQ 0265-6736 Google Scholar
O. Dahl, Hyperthermia and Oncology, 29
–39 VSP, Utrecht, The Netherlands
(1994). Google Scholar
G. M. Hahn, J. Braun and I. Har-Kedar,
“Thermochemotherapy: synergism between hyperthermia (42–43 degrees) and adriamycin (or bleomycin) in mammalian cell inactivation,”
937
–940
(1975). http://dx.doi.org/10.1073/pnas.72.3.937 Google Scholar
J. Michalakis, S. D. Georgatos and E. Bree,
“Short-term exposure of cancer cells to micromolar doses of paclitaxel, with or without hyperthermia, induces long-term inhibition of cell proliferation and cell death in vitro,”
Ann. Surg. Oncol., 14
(3), 1220
–1228
(2007). http://dx.doi.org/10.1245/s10434-006-9305-4 Google Scholar
H. H. Kampinga and E. Dikomey,
“Hyperthermic radiosensitization: mode of action and clinical relevance,”
Int. J. Radiat. Biol., 77 399
–408
(2001). http://dx.doi.org/10.1080/09553000010024687 IJRBE7 0955-3002 Google Scholar
H. Park et al.,
“Multifunctional nanoparticles for combined doxorubicin and photothermal treatments,”
ACS Nano, 3
(10), 2919
–2926
(2009). http://dx.doi.org/10.1021/nn900215k ANCAC3 1936-0851 Google Scholar
W. Zhang et al.,
“Synergistic effect of chemo-photothermal therapy using PEGylated graphene oxide,”
Biomaterials, 32
(33), 8555
–8561
(2011). http://dx.doi.org/10.1016/j.biomaterials.2011.07.071 BIMADU 0142-9612 Google Scholar
J. G. Mehtala et al.,
“Synergistic effects of cisplatin chemotherapy and gold nanorod-mediated hyperthermia on ovarian cancer cells and tumors,”
Nanomedicine, 9
(13), 1939
–55
(2014). http://dx.doi.org/10.2217/nnm.13.209 1743-5889 Google Scholar
Y. Tang and A. J. McGoron,
“Combined effects of laser-ICG photothermotherapy and doxorubicin chemotherapy on ovarian cancer cells,”
J. Photochem. Photobiol. B, 97 138
–144
(2009). http://dx.doi.org/10.1016/j.jphotobiol.2009.09.001 JPPBEG 1011-1344 Google Scholar
S. J. Oldenburg et al.,
“Infrared extinction properties of gold nanoshells,”
Appl. Phys. Lett., 75 2897
–2899
(1999). http://dx.doi.org/10.1063/1.125183 APPLAB 0003-6951 Google Scholar
X. P. Huang et al.,
“Gold nanoparticles: interesting optical properties and recent applications in cancer diagnostics and therapy,”
Nanomedicine, 2 681
–693
(2007). http://dx.doi.org/10.2217/17435889.2.5.681 1743-5889 Google Scholar
H. Maeda,
“Toward a full understanding of the EPR effect in primary and metastatic tumors as well as issues related to its heterogeneity,”
Adv. Drug Delivery Rev., 91 3
–6
(2015). http://dx.doi.org/10.1016/j.addr.2015.01.002 ADDREP 0169-409X Google Scholar
E. Huynh and G. Zheng,
“Cancer nanomedicine: addressing the dark side of the enhanced permeability and retention effect,”
Nanomedicine, 10
(13), 1993
–1995
(2015). http://dx.doi.org/10.2217/nnm.15.86 1743-5889 Google Scholar
M. A. Fischbach, J. A. Bluestone and W. A. Lim,
“Cell-based therapeutics: the next pillar of medicine,”
Sci. Transl. Med., 5
(179), 7
(2013). http://dx.doi.org/10.1126/scitranslmed.3005568 STMCBQ 1946-6234 Google Scholar
M. T. Basel et al.,
“Cells as delivery vehicles for cancer therapeutics,”
Ther. Delivery, 5
(5), 555
–567
(2014). http://dx.doi.org/10.4155/tde.14.24 Google Scholar
S. Valable et al.,
“In vivo MRI tracking of exogenous monocytes/macrophages targeting brain tumors in a rat model of glioma,”
Neuroimage, 40 973
–983
(2008). http://dx.doi.org/10.1016/j.neuroimage.2008.01.005 NEIMEF 1053-8119 Google Scholar
M. T. Basel et al.,
“Cell-delivered magnetic nanoparticles caused hyperthermia-mediated increased survival in a murine pancreatic cancer model,”
Int. J. Nanomedicine, 7 297
–306
(2012). http://dx.doi.org/10.2147/IJN.S28344 Google Scholar
M. R. Choi et al.,
“Delivery of nanoparticles to brain metastases of breast cancer using a cellular Trojan horse,”
Cancer Nanotechnol., 3 47
–54
(2012). http://dx.doi.org/10.1007/s12645-012-0029-9 Google Scholar
J. Fu et al.,
“Macrophage mediated biomimetic delivery system for the treatment of lung metastasis of breast cancer,”
J. Control. Release, 204 11
–19
(2015). http://dx.doi.org/10.1016/j.jconrel.2015.01.039 Google Scholar
M. R. Choi et al.,
“A cellular Trojan horse for delivery of therapeutic nanoparticles into tumors,”
Nano Lett., 7
(12), 3759
–3765
(2007). http://dx.doi.org/10.1021/nl072209h Google Scholar
S. K. Baek et al.,
“Photothermal treatment of glioma: an in vitro study of macrophage-mediated delivery of gold nanoshells,”
J. Neurooncol., 104 439
–448
(2011). http://dx.doi.org/10.1007/s11060-010-0511-3 Google Scholar
S. J. Madsen et al.,
“Nanoparticle-loaded macrophage-mediated photothermal therapy: potential for glioma treatment,”
Lasers Med. Sci., 30
(4), 1357
–1365
(2015). http://dx.doi.org/10.1007/s10103-015-1742-5 Google Scholar
C. Christie et al.,
“Macrophages as nanoparticle delivery vectors for photothermal therapy of brain tumors,”
Ther. Delivery, 6
(3), 371
–384
(2015). http://dx.doi.org/10.4155/tde.14.121 Google Scholar
J. A. Schwartz et al.,
“Feasibility study of particle-assisted laser ablation of brain tumors in orthotopic canine model,”
Cancer Res., 69 1659
–1667
(2009). http://dx.doi.org/10.1158/0008-5472.CAN-08-2535 CNREA8 0008-5472 Google Scholar
B. Drewinko et al.,
“Combination chemotherapy in vitro with adriamycin. Observation of additive, antagonistic and synergistic effects when used in two-drug combinations on cultured human lymphoma cells,”
Cancer Biochem. Biophys., 1
(4), 187
–195
(1976). CABCD4 Google Scholar
R. Goldman,
“Effect of retinoic acid on the proliferation and phagocytic capability of murine macrophage-like cell lines,”
J. Cell. Phys., 120 91
–102
(1984). http://dx.doi.org/10.1002/jcp.1041200113 Google Scholar
L. R. Hirsch et al.,
“Nanoshell-mediated near-inrared thermal therapy of tumors under magnetic resonance guidance,”
13549
–13554
(2003). http://dx.doi.org/10.1073/pnas.2232479100 Google Scholar
A. Trinidad et al.,
“Combined concurrent photodynamic and gold nanoshell loaded macrophage-mediated photothermal therapies: an in vitro study on squamous cell head and neck carcinoma,”
Lasers Surg. Med., 46 310
–318
(2014). http://dx.doi.org/10.1002/lsm.22235 LSMEDI 0196-8092 Google Scholar
S. Chhetri, H. Hirschberg and S. J. Madsen,
“Photothermal therapy of human glioma spheroids with gold-silica nanoshells and gold nanorods: a comparative study,”
Proc. SPIE, 8928 89280U
(2014). http://dx.doi.org/10.1117/12.2038233 Google Scholar
G. Sahay, D. Y. Alakhova and A. V. Kabanov,
“Endocytosis of nanomedicines,”
J. Control. Release, 145 182
–195
(2010). http://dx.doi.org/10.1016/j.jconrel.2010.01.036 JCREEC 0168-3659 Google Scholar
H. Kim et al.,
“Photothermally triggered cytosolic drug delivery via endosome disruption using a functionalized reduced graphene oxide,”
ACS Nano, 7 6735
–6746
(2013). http://dx.doi.org/10.1021/nn403096s ANCAC3 1936-0851 Google Scholar
D. Ma,
“Enhancing endosomal escape for nanoparticle mediated siRNA delivery,”
Nanoscale, 6 6415
–6425
(2014). http://dx.doi.org/10.1039/c4nr00018h NANOHL 2040-3364 Google Scholar
|