|
|
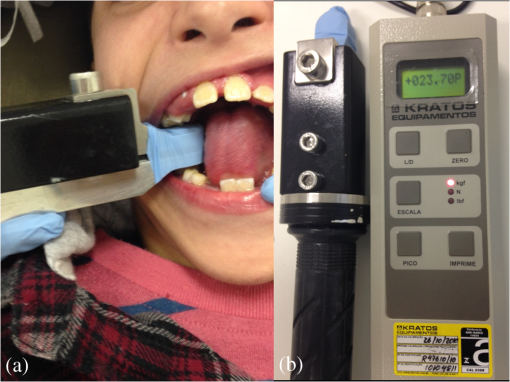
1.IntroductionCerebral palsy (CP) describes a group of chronic disorders that affect movement and posture development, often accompanied by epilepsy, secondary musculoskeletal problems, and disturbances of sensation, perception, cognition, communication, and behavior. It is the most common cause of severe physical disability during childhood,1 with an estimated prevalence of children.2 Muscle spasticity is the most common musculoskeletal problem. It is defined as a velocity-dependent resistance to passive stretch, and is clinically assessed using the modified Ashworth scale.3 It predominantly affects the antigravity muscles, and causes an increase in the deep reflex and muscle tone.4 Upon injury to the central nervous system, as occurs in individuals with CP, neural reorganization causes an adaptive but pathological change in peripheral muscle control. The result is a diminished inhibition of muscle contraction and a hyperactive reflex arc that is triggered by muscle stretch.4,5 Muscle spasticity acts as a negative factor in the functioning of the masticatory masseter and temporalis muscles, causing hypertonia of these muscles. This limits the amplitude opening of the mouth, resulting in difficulties in feeding and performing oral hygiene procedures. The interposition of the soft tissue between the dental arches during muscle spasms results in soft tissue trauma due to the lack of protective reflexes caused by the mandibular movement disorders resulting from the muscle spasticity.6 The biophysical attributes of low-intensity laser radiation open up new dimensions in their therapeutic applications used in a variety of clinical procedures.7–9 Low-level laser therapy (LLLT) promotes analgesia;7 has positive effects in the treatment of fatigue, pain, and fibromyalgia;10–12 and improves the muscle repair process.13 Additionally, LLLT can modulate nerve impulses. It has been stated that LLLT reduces the electrical excitability of cultured nerve cells.14 A double-blind study in humans reported a reduction of the clonus in individuals with spinal cord injuries after LLLT, an effect identical to that observed after peripheral electrical nerve stimulation.15 The irradiation of the skin overlying the median nerve in humans also mimics the effects of the electric stimulation of the same nerve, which results in a large decrease in the amplitude of the evoked electrical potential.16 Experiments in rats, however, have been reported to produce different results. Laser irradiation was reported to increase the action potential after a single dose of transcutaneous irradiation.17 The isolated sciatic nerves of frogs were found to have only an increased latency in their compound-action potential amplitude.18 Previous studies have described the potential use of LLLT in the treatment of limb and trunk spasticity in individuals with CP, indicating a promising treatment modality that might improve their quality of life.19,20 However, to our knowledge, no studies regarding the effects of LLLT on oral muscle spasticity in subjects with CP have been reported in literature. With this perspective, the aim of this study was to determine the effect of LLLT on the spasticity of the masseter and anterior temporal muscle fibers of children with CP by evaluating the changes in the amplitude of mouth opening and the bite force of the masticatory muscles over a 3-week intermittent application period. Our hypothesis was that LLLT would improve the amplitude of mouth opening and reduce the bite force in individuals with CP. 2.Materials and MethodsThis study was approved by the Research Ethics Committee of the Cruzeiro do Sul University, São Paulo, Brazil (#094/2011). Written informed consent for participation and publication was obtained from the adult caregiver responsible for each patient who agreed to participate. 2.1.Study DesignA longitudinal study was conducted with children who were referred to a specialized rehabilitation center in São Paulo, Brazil. 2.2.SubjectsThirty noninstitutionalized, 8- to 14-year-old male and female children with a medical diagnosis of spastic CP were included in this study. For their inclusion in this study, the children had to present the ability to follow verbal instructions and were required to be cooperative. The exclusion criteria were the use of analgesics, antiinflammatory, and antispasmodic medications; application of the botulinum toxin (BTX) type A injection in the masticatory muscles in the three months preceding data collection; the presence of oral or dental pain; and the use of orthodontic appliances. 2.3.Bite Force MeasurementAn electronic dynamometer (model DMD Kratos Equipments, São Paulo, Brazil) was used to measure the bite force (BF) before and after laser irradiation during the three weeks of LLLT exposures as well as once a week during the subsequent 3-week clinical followup. The BF was measured with the dynamometer positioned between the upper and lower permanent first molar for the mixed or permanent dentition types (Fig. 1). The measurements were performed bilaterally. A short training period was conducted prior to the initiation of the tests to prepare the patients for the proposed activities. Theoretical explanations concerning the procedures and the dynamometry placement were provided, and the subjects were trained to bite as hard as possible. After this, each individual was asked to bite the apparatus for 5 s; this procedure was repeated three times with 2-min intervals between bites. The highest peak value registered among the three trials was considered to be the individual’s BF measurement, recorded in Kgf. 2.4.Measurement of the Amplitude of Mouth OpeningThe patients were asked to open their mouth to the maximum amplitude possible, and the amplitude was measured using a caliper, such that the stems of the caliper touched the incisal face of the upper and lower central incisors.21 2.5.Low-Intensity Laser IrradiationThe masseter and temporalis muscles on both sides of the face were irradiated in the middle of each muscle for three consecutive weeks: three times in week 1, on alternate days (Monday/Wednesday/Friday); twice in week 2 (Monday/Wednesday); and once in week 3 (Monday). Laser irradiation was performed with a continuous wave (CW) infrared low-level Ga–Al–As laser (, 120 mW; Twin Flex Evolution Laser MMOptics, São Paulo, Brazil) using a energy dose per site, with a 20-s exposure time per site (spot area: ; irradiance: ; energy delivery per point: 2.4 J). The parameters of the LLLT application were determined based on a previous study regarding the use of a low-potency diode, InGaAlP, applied for the treatment of traumatic labial injury in patients with spastic cerebral palsy, which allowed a 24-h interval between the first and second administration and a 7-day interval between the two subsequent ones.22 All of the clinical examinations were performed by the same calibrated examiner (Fernando Martins Baeder), who assessed the muscle spasticity by palpation by a 2-s application of pressure, in accordance with the diagnostic criteria for temporomandibular disorders (DC/TMD).23 The exact point of LLLT irradiation on the muscles for each of the patients was selected based on the point of the greatest contraction observed upon palpation. One point on each muscle was treated in each of the LLLT sessions; a total of six sessions were conducted over three weeks. The amplitude of mouth opening and the bite force were recorded before and immediately after each of the LLLT sessions, and again during the following three weeks of clinical followup, when laser therapy was not performed. 2.6.Statistical AnalysisThe data for the bite force and the amplitude of mouth opening over the 6-week experimental period were tabulated and processed using the statistical software program MedCalc for Windows, version 14.8.1 (Mariakerke, Belgium). The selected level of statistical significance adopted was 95%. Statistical analyses were performed using nonparametric assessments. The Wilcoxon test was applied for the comparison of the mean values prior to and following laser irradiation sessions during the three weeks of LLLT application. The Friedman and multiple comparisons tests were used for the comparison of the mean values obtained after each of the sessions of the study. A was considered to indicate a statistically significant difference between the pre- and postlaser measurements within each week and over the 6-week period. 3.ResultsThirty children with medically diagnosed spastic CP were enrolled in this study. The sample population consisted of 19 male (63.3%) and 11 female (36.7%) patients, ranging in age from 6 to 13 years old (). Five of the children had spastic diplegic CP (16.7%), two had hemiplegic CP (6.7%), and 23 had quadriplegic CP (76.6%). A significant difference was observed between the mean values of the BF and the amplitude of mouth opening before and after irradiation within the 3-week duration of the study (). Statistical differences were also observed among the six sessions pre- and postlaser irradiation () (Table 1). Table 1Mean values and standard deviation of the bite force (Kgf) and the amplitude of mouth opening (mm) prior and following laser irradiation sessions during the three weeks of LLLT application.
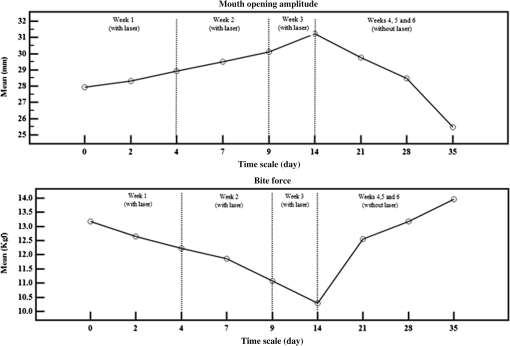
A decrease in the BF and an increase in the amplitude of mouth opening were noticed up to week 3 of LLLT application (Fig. 2). However, there were no differences between the values of these parameters recorded at week 6 and those obtained prior to the first laser irradiation. The BF values at week 6 and prior to the first irradiation were and , respectively (); the values of the amplitude of mouth opening at week 6 and prior to the first irradiation were and , respectively (). 4.DiscussionSeveral pharmacological and nonpharmacological treatments are used to treat spasticity in individuals with CP. However, most of the pharmacological treatment options are known to cause undesirable side effects.6,24,25 Literature regarding the treatment of spasticity in the masticatory muscle in CP is scarce.6 Laser therapy has been proven to accelerate muscle recovery26 and prevent the damage induced by the metabolic disturbances and inflammatory reactions following heavy exercise.25 Therefore, the present investigation aimed to evaluate the efficacy of LLLT in spasticity control in patients with CP. To our knowledge, this is the first report of the evaluation of the therapeutic effect of LLLT on the spastic masticatory muscles of individuals with CP. Our study demonstrated that LLLT is an effective noninvasive therapeutic modality capable of promoting relaxation in spastic masticatory muscles, resulting in a reduction in the BF and an increase in the amplitude of mouth opening in children with spastic CP. Although the modified Ashworth scale3 is usually used to clinically assess the level of the spastic tonus, none of the studies in literature report the use of the same or any other relevant scale for the evaluation of the levels of spasticity of the masseter or temporalis muscles. Nevertheless, the increase in the amplitude of mouth opening and the decrease in the muscle tonus in individuals with spastic CP have been described in literature as diagnostic parameters for the evaluation of the therapeutic effects of cryotherapy21 and BTX6 on spasticity. According to the new DC/TMD,23 the types of myalgia are differentiated by provocation testing with palpation, and can be classified as local myalgia, myofascial pain, and myofascial pain with referral. In this study, this system of classification was used as the criteria for the diagnosis of local myalgia (ICD-9 729.1; ICD-10 M79.1) by clinical examination, along with the confirmation of pain in the temporalis and masseter muscles or report of pain in the site of palpation. In a previous study by our group,6 the points of injection of BTX-A in children with spastic CP were determined by palpation. This injection was applied at the site of the greatest contraction of the masseter and temporal muscles, which was generally located in the middle of each muscle. The same principle was used in this pioneer study. However, more studies are needed to evaluate other points of application for LLLT. Our results are in agreement with a previous study that demonstrated the reduction of clonus in humans.15 It can be speculated that the same mechanism was in operation in our study too—a decrease in the amplitude of the electrically evoked potential.16 The laser irradiation was performed with an energy density of at each point, with a higher muscular palpation contraction in the middle of the selected muscles, for a duration of 20 s per site over six applications (Day 0 to 14). These parameters are in agreement with a previous study that demonstrated that 6 to 10 applications of low-intensity laser irradiation were enough to increase the metabolic pattern of the muscle fibers,27 and also with other basic studies on LLLT that have demonstrated the greatest therapeutic effectiveness when the laser source is in contact with the biological tissue in conventional exposures at selected points for 20 to 30 s.28 The frequent intense use of muscles during high-intensity exercise or during repeated muscle contractions leads to a decrease in the muscle performance and causes the appearance of peripheral muscle fatigue.10 This condition can also result from a diminished inhibition of muscle contraction and a hyperactive reflex arc that is triggered by muscle stretch, as seen in spastic muscles.4,5 Muscle contraction depends on the electrical excitation of the muscle fibers. This contraction involves the release of , which is directly linked to the (voltage-dependent) and [adenosine triphosphate (ATP)-dependent] channels in the sarcolemma and T-tubules. Repeated muscle contraction has been associated with the induction of fatigue because it promotes an increased influx and efflux from the muscle cells.29 It is possible that LLLT influences the excitation of the muscle fibers and reduces muscle fatigue by indirectly modulating the pump, which is ATP-dependent. The ATP synthesis by the mitochondria surrounding the T-tubules and cisterns might increase as a result of LLLT. The greater availability of ATP might improve the function of the pump and prevent an extracellular accumulation of ;29 this could be one of the possible explanations of the reduction in the BF and the increase in the amplitude of mouth opening observed in this study. In fact, LLLT reduces muscle fatigue during tetanic contractions and reduces muscle damage, as inferred by the reduction in the plasma creatine kinase levels.25 The cytochrome C oxidase activity is enhanced by LLLT in vivo, thus promoting the higher availability of ATP and the storage of energy in muscle cells exclusively by the adenosine triphosphate-creatine phosphate (phosphagen system) bioenergetic system.30 It is possible that LLLT might have a more extensive and complex mechanism of muscle cell modulation, as demonstrated by the delaying of the progression of dystrophy in a previous study.31 One limitation of this study is related to the absence of protocols available concerning the application of LLLT for the treatment of spasticity in masticatory muscles in subjects with cerebral palsy. The time scale of the LLLT application was selected based on the limitations in the attendance of the children with cerebral palsy at the treatment center, since the patients need special assistance for their transportation from home to the rehabilitation center and, also, the caregivers need to assume the responsibility to follow of all of the prescribed health and support therapies. In addition, the majority of these children were severely distressed during the treatment, presenting stress episodes with tachycardia because they were not in their accustomed environment. One of the questions addressed in this study was regarding the duration for which the spastic muscular cells would retain the effects of LLLT following the initial six sessions of irradiation. This was determined by performing the evaluations without laser application during a subsequent 3-week followup. A reduction in the efficacy of the laser therapy was observed after one week without LLLT application, which was further accentuated after two weeks. The values of the evaluated parameters returned to the initial preapplication values after three weeks. The caregivers reported an improvement in sleeping, sucking, and swallowing in the children during a period of 15 days after the last application of LLLT, thereby indicating that the therapy might also be helpful in improving the oral hygiene performance. These results suggest that after the initial six LLLT applications, weekly applications should be instituted to maintain the beneficial effects achieved. Further research is required to determine the ideal interval between sessions to maintain the long-term efficacy of LLLT. It should be stressed that the findings of the present investigation are of importance to dental surgeons who treat individuals with spastic CP for dental problems, since they show that LLLT promotes the increase of the amplitude of mouth opening and decrease of the muscular tonus. Low levels of energy exposures of 808-nm CW diode laser were shown to be an effective short-term therapeutic tool to increase the amplitude of mouth opening and decrease the muscle tonus of children with spastic CP upon application over a period of three weeks. AcknowledgmentsThis study was supported by the São Paulo Research Foundation (“Fundação de Amparo a Pesquisa do Estado de São Paulo,” FAPESP—#10/52427-0). ReferencesP. Rosenbaum et al.,
“A report: the definition and classification of cerebral palsy April 2006,”
Dev. Med. Child. Neurol. Suppl., 109 8
–14
(2007). Google Scholar
D. Hirtz et al.,
“How common are the common neurologic disorders?,”
Neurology, 68
(5), 326
–337
(2007). http://dx.doi.org/10.1212/01.wnl.0000252807.38124.a3 NEURAI 0028-3878 Google Scholar
R. W. Bohannon and M. B. Smith,
“Interrater reliability of a modified Ashworth scale of muscle spasticity,”
Phys. Ther., 67
(2), 206
–207
(1987). POTPDY Google Scholar
J. M. Gracies,
“Pathophysiology of spastic paresis. I: paresis and soft tissue changes,”
Muscle Nerve, 31
(5), 535
–551
(2005). http://dx.doi.org/10.1002/mus.20284 Google Scholar
J. M. Gracies,
“Pathophysiology of spastic paresis. II: emergence of muscle overactivity,”
Muscle Nerve, 31
(5), 552
–571
(2005). http://dx.doi.org/10.1002/mus.20285 Google Scholar
F. S. Manzano et al.,
“Treatment of muscle spasticity in patients with cerebral palsy using BTX-A: a pilot study,”
Spec. Care Dent., 24
(4), 235
–239
(2004). http://dx.doi.org/10.1111/j.1754-4505.2004.tb01699.x Google Scholar
V. H. Panhoca et al.,
“Comparative clinical study of light analgesic effect on temporomandibular disorder (TMD) using red and infrared led therapy,”
Lasers Med. Sci., 30
(2), 815
–822
(2015). http://dx.doi.org/10.1007/s10103-013-1444-9 Google Scholar
J. Tunér and L. Hode, The Laser Therapy Handbook: A Guide for Research Scientists, Doctors, Dentists, Veterinarians and Other Interested Parties Within the Medical Field, Prisma, Stockholm, Sweden
(2004). Google Scholar
R. Waynant and D. B. Tata, Proceedings of Light-Activated Tissue Regenaration and Therapy Conference, Springer, Boston, MA
(2008). Google Scholar
F. A. Dos Reis et al.,
“Effects of pre- or post-exercise low-level laser therapy (830 nm) on skeletal muscle fatigue and biochemical markers of recovery in humans: double-blind placebo-controlled trial,”
Photomed. Laser Surg., 32
(2), 106
–112
(2014). http://dx.doi.org/10.1089/pho.2013.3617 Google Scholar
A. F. Oton-Leite et al.,
“Effect of low level laser therapy in the reduction of oral complications in patients with cancer of the head and neck submitted to radiotherapy,”
Spec. Care Dent., 33
(6), 294
–300
(2013). http://dx.doi.org/10.1111/j.1754-4505.2012.00303.x Google Scholar
A. Carbonell-Baeza et al.,
“Multidisciplinary and biodanza intervention for the management of fibromyalgia,”
Acta Reumatol. Port., 37
(3), 240
–250
(2012). Google Scholar
R. V. Gonçalves et al.,
“Time-dependent effects of low-level laser therapy on the morphology and oxidative response in the skin wound healing in rats,”
Lasers Med. Sci., 28
(2), 383
–390
(2013). http://dx.doi.org/10.1007/s10103-012-1066-7 Google Scholar
J. E. Olson, W. Schimerling and C. A. Tobias,
“Laser action spectrum of reduced excitability in nerve cells,”
Brain Res., 204
(2), 436
–440
(1981). http://dx.doi.org/10.1016/0006-8993(81)90604-1 BRREAP 0006-8993 Google Scholar
J. B. Walker,
“Temporary suppression of clonus in humans by brief photostimulation,”
Brain Res., 340
(1), 109
–113
(1985). http://dx.doi.org/10.1016/0006-8993(85)90779-6 BRREAP 0006-8993 Google Scholar
J. B. Walker and L. K. Akhanjee,
“Laser-induced somatosensory evoked potentials: evidence of photosensitivity in peripheral nerve,”
Brain Res., 344
(2), 281
–285
(1985). http://dx.doi.org/10.1016/0006-8993(85)90805-4 BRREAP 0006-8993 Google Scholar
S. Rochkind et al.,
“Response of peripheral nerve to He-Ne laser: experimental studies,”
Lasers Surg. Med., 7
(5), 441
–443
(1987). http://dx.doi.org/10.1002/lsm.1900070512 LSMEDI 0196-8092 Google Scholar
D. W. Ebert and C. Roberts,
“In vitro frog sciatic nerve as a peripheral nerve model for studies of the mechanism of action of low energy lasers: part one,”
Lasers Surg. Med., 21
(1), 32
–41
(1997). http://dx.doi.org/10.1002/(SICI)1096-9101(1997)21:1<32::AID-LSM6>3.0.CO;2-Z LSMEDI 0196-8092 Google Scholar
Y. Asagai et al.,
“Application of low reactive-level laser therapy (LLLT) in the functional training of cerebral palsy patients,”
Laser Ther., 6
(4), 195
–201
(1994). http://dx.doi.org/10.5978/islsm.94-OR-14 LATHE5 0898-5901 Google Scholar
Y. Asagai et al.,
“Application of low reactive-level laser therapy (LLLT) in patients with cerebral palsy of the adult tension athetosis type,”
Laser Ther., 7
(3), 113
–118
(1995). http://dx.doi.org/10.5978/islsm.95-OR-15 LATHE5 0898-5901 Google Scholar
M. T. dos Santos and L. M. de Oliveira,
“Use of cryotherapy to enhance mouth opening in patients with cerebral palsy,”
Spec. Care Dentist., 24
(4), 232
–234
(2004). http://dx.doi.org/10.1111/j.1754-4505.2004.tb01698.x Google Scholar
L. A. Moreira et al.,
“Efficiency of laser therapy applied in labial traumatism of patients with spastic cerebral palsy,”
Braz. Dent. J., 15
(Spec No), SI29
–S33
(2004). Google Scholar
E. Schiffman et al.,
“Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network* and orofacial pain special interest group,”
J. Oral Facial Pain Headache., 28
(1), 6
–27
(2014). http://dx.doi.org/10.11607/jop.1151 Google Scholar
C. Y. Chung et al.,
“Pharmacotherapy of spasticity in children with cerebral palsy,”
J. Formos. Med. Assoc., 110
(4), 215
–222
(2011). http://dx.doi.org/10.1016/S0929-6646(11)60033-8 JFASEO 0929-6646 Google Scholar
E. C. Leal Junior et al.,
“Effect of 830 nm low-level laser therapy applied before high-intensity exercises on skeletal muscle recovery in athletes,”
Lasers Med. Sci., 24
(6), 857
–863
(2009). http://dx.doi.org/10.1007/s10103-008-0633-4 Google Scholar
E. C. Leal-Junior et al.,
“Effect of phototherapy (low-level laser therapy and light-emitting diode therapy) on exercise performance and markers of exercise recovery: a systematic review with meta-analysis,”
Lasers Med Sci., 30
(2), 925
–939
(2015). http://dx.doi.org/10.1007/s10103-013-1465-4 Google Scholar
É. C. Rizzi et al.,
“Low-level laser intensity application in masseter muscle for treatment purposes,”
Photomed. Laser Surg., 28
(Suppl 2), S31
–S35
(2010). http://dx.doi.org/10.1089/pho.2009.2599 Google Scholar
J. M. Bjordal et al.,
“Low-level laser therapy in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials,”
Photomed. Laser Surg., 24
(2), 158
–168
(2006). http://dx.doi.org/10.1089/pho.2006.24.158 Google Scholar
O. B. Nielsen and F. V. de Paoli,
“Regulation of homeostasis and excitability in contracting muscles: implications for fatigue,”
Appl. Physiol. Nutr. Metab., 32
(5), 974
–984
(2007). http://dx.doi.org/10.1139/H07-099 Google Scholar
G. M. Albuquerque-Pontes et al.,
“Effect of pre-irradiation with different doses, wavelengths, and application intervals of low-level laser therapy on cytochrome c oxidase activity in intact skeletal muscle of rats,”
Lasers Med. Sci., 30
(1), 59
–66
(2015). http://dx.doi.org/10.1007/s10103-014-1616-2 Google Scholar
E. C. Leal-Junior et al.,
“Superpulsed low-level laser therapy protects skeletal muscle of mdx mice against damage, inflammation and morphological changes delaying dystrophy progression,”
PLoS One, 9
(3), e89453
(2014). http://dx.doi.org/10.1371/journal.pone.0089453 POLNCL 1932-6203 Google Scholar
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||