|
|
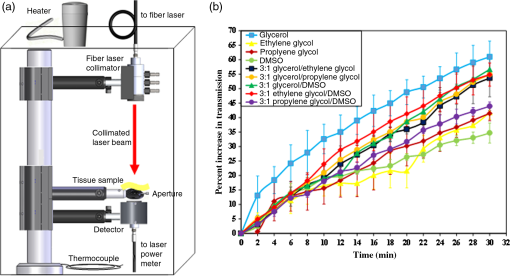
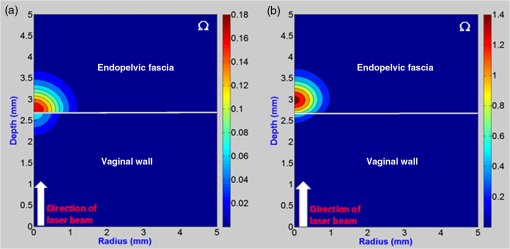
1.Introduction1.1.Female Stress Urinary IncontinenceOver 6.5 million women in the United States suffer from stress urinary incontinence (SUI), but only 3% of these women choose to have surgery.1,2 General anesthesia, long recovery time, surgical incisions, potential treatment failures associated with future pregnancy, and morbidity of the procedure are several common reasons provided by patients who are reluctant to have surgery. The vast majority of women instead use disposable absorbable products to cope with their symptoms.3 A nonsurgical method that improves patient quality of life, that can be rapidly performed, has minimal morbidity, and only a short recovery time may prove to be a desirable alternative for treatment of female SUI. 1.2.Preliminary Laser StudiesOur preliminary studies showed that subsurface thermal tissue denaturation can be achieved using deeply penetrating near-infrared laser energy in combination with applied cooling, to preserve 1 to 2 mm of tissue surface from thermal insult.4,5 For SUI treatment, the goal is to thermally remodel and tighten endopelvic fascia without damaging surrounding tissue layers (e.g., urethra or vaginal wall). The thickness of the vaginal wall, endopelvic fascia, and urethral wall has been measured with ultrasound to be 2.7, 4.3, and 2.4 mm, respectively.6,7 The vaginal wall may potentially be preserved while submucosal tissue is thermally remodeled, using an endoscopic laser probe with integrated cooling for minimally invasive treatment of SUI. Recent computer simulations of light transport, heat transfer, and tissue thermal damage have demonstrated that a transvaginal approach is more feasible than a transurethral approach.8 However, results were suboptimal, and some undesirable thermal insult to the vaginal wall was still predicted. 1.3.Optical Clearing AgentsOptical clearing agents (OCAs) have been used for reducing light scattering and increasing optical penetration depth in tissues for optical diagnostics (e.g., imaging and spectroscopy) and laser therapy.9–15 Optical clearing is achieved through both refractive-index matching and tissue dehydration.16 The OCA induces water flux from the interstitial space to the tissue surface, and the increase in osmolarity of interstitial fluid draws water from the cell and leads to dehydration.17 These processes provide additional refractive-index matching and a decrease in the reduced scattering coefficient for skin. Decreased scattering may significantly enhance optical transmission, which in turn translates into improved optical penetration depth. Optical clearing has been successfully demonstrated in a wide range of tissues including skin,15,18,19 muscle,16 collagen,20 cartilage,21 and bone22 using different agents and concentrations. For example, recent studies in skin, in vitro, have shown a 53% increase in transmission.18 In general, higher concentrations and longer immersion times yield higher optical transmission. In some cases, however, improved optical transmission does not correspond to highest concentration. For example, 70% glycerol concentration has been reported to provide deeper light penetration than 90% glycerol in porcine skin.23 Similarly, an optimal diffusion concentration of 40.5% with glucose and ethylene glycol (EG) mixture instead of higher concentration of EG has been reported. This superior result obtained with a lower OCA concentration is likely to do with the better equilibrium between tissue free-water content and the water in the treatment solution, which yields a maximum agent diffusion rate.24 The primary objective of this study is to determine whether application of an OCA will allow deeper targeting of endopelvic fascia for laser thermal remodeling with complete preservation of the vaginal wall from thermal insult. 2.MethodsSeveral experimental methods were used in our experiments. In those methods, which are described in detail in the following sections, we have used porcine vaginal tissues with the physical data provided in Table 1. Table 1Optical, thermal, and damage parameters for computer simulations of transvaginal and transurethral laser therapy. A laser wavelength of 1064 nm, incident power of 5.0 W, spot diameter of 5.0 mm, and irradiation time of 15 s was used.
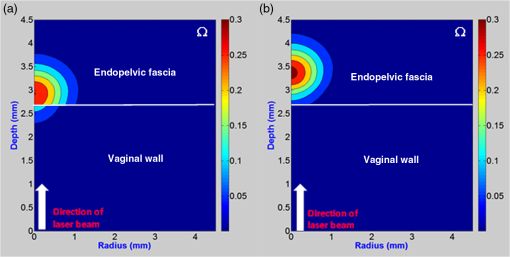
2.1.Optical Clearing AgentsOCAs are commonly mixed with other solutions, for example, dimethyl sulfoxide (DMSO), to enhance the rate of perfusion into tissue.30–32 Our laboratory reported a 26% increase in transmission through canine skin using a mixture of glycerol/DMSO.33 Other mixtures of OCA’s and transport agents have also been tested, including propylene glycol (PG) and EG. For these studies in porcine vaginal tissue, a minimum of three measurements were performed for each type of the following OCA mixtures tested: 100% glycerol (), 100% PG (), 100% EG (), 100% DMSO (), glycerol/DMSO (), glycerol/PG (), glycerol/EG (), PG/DMSO (), and EG/DMSO (). 2.2.Experimental Setup for Measuring Percent Change in Optical TransmissionFresh porcine vaginal tissues were obtained from Spear Products, Inc. (Coopersburg, Pennsylvania). The tissue was stored in saline and refrigerated for use within 48 h. A continuous-wave ytterbium fiber laser at 1075-nm wavelength and with a collimated beam diameter of 5.2 mm () was used. A heat chamber maintained consistent temperature (37°C), and initial intensity was measured before OCA was applied. After OCA application to porcine vaginal tissue, transmitted power was recorded from a detector (PM10, Molectron, Portland, Oregon) connected to a power meter (EPM1000, Molectron) every 2 min for a period of 30 min. 2.3.Optical Coherence TomographyOptical coherence tomography (OCT) of vaginal tissue with and without OCA was performed with an OCT system (Niris, Imalux, Cleveland, Ohio) and a handheld 8 Fr probe. The OCT system was a time-domain system based on a common path all fiber interferometer design and operated at a wavelength of 1300 nm, acquiring images with axial resolution and lateral resolution. OCT images of vaginal tissue before and after application of glycerol were acquired to determine increased image depth based on decreased tissue scattering. Measurements were performed using imageJ software (National Institutes of Health, Bethesda Maryland) to analyze the 256 gray scale images. 2.4.Reflection SpectroscopyA spectrometer was used to quantify the change in reflection spectrum of porcine vaginal wall as a function of OCA application time. A fiber optic cable (RP21, Thorlabs, Newton, New Jersey) was used to connect both the white light source (MI-150, Edmund Optics, Barrington, New Jersey) and the spectrometer (USB 4000-VIS-NIR, Ocean Optics, Dunedin, Florida). The fiber tip was in direct contact with the sample, and reflectance data were collected using the proprietary software, Spectra Suite (ocean optics). By comparing the baseline spectrum from native tissue at 0 min with the spectrum from optically cleared tissue, the percentage change in reflection spectrum due to OCA was calculated. 2.5.Computer SimulationsUsing experimental data on change in transmission by OCA in a known thickness of porcine vaginal tissue, change in scattering and absorption can be determined. Using Beer–Lambert law, where is the attenuation coefficient (), is the absorption coefficient (), is the scattering coefficient (), is the anisotropy factor measuring directional scattering, is the tissue thickness (cm), is the initial laser intensity (), is the intensity measured through porcine vaginal tissue at 0 min, and is the intensity measured through tissue after 30 min of OCA topical application.A decrease in the reduced scattering coefficient, defined as , is the dominant OCA effect.34 The simulations assume that the absorption coefficient and anisotropy factor remain constant and that only the scattering coefficient changes upon OCA application. This calculation reduces the scattering coefficient from 21.6 to as shown below and used in Table 1. From Eq. (2) above, the following calculation is performed: Combining this expression with Eq. (3) results in the following expression: Since absorption coefficient and anisotropy factor are unchanged, the equation simplifies to where , , , .Substituting these values into the equation yields a scattering coefficient of . Optical clearing potential (OCP) is defined as a ratio of (before) and (after) [Eq. (4)]. For human skin, glycerol was previously reported to have an average OCP of 3;19 in this study, glycerol applied to vaginal wall produced a similar OCP of 3.6. where is reduced scattering coefficient () given by ().A Monte Carlo (MC) program was adapted to simulate the distribution of 1 million photons absorbed in tissue layers.35–37 A convolution program fitted results to a laser beam of known power, profile, and diameter.37 Values for tissue optical properties were compiled based on the Nd:YAG laser wavelength used in previous experimental studies (Table 1). Temperature simulations were conducted using finite element software (ANSYS 14.5). A heat transfer model was imported from MC model dimensions with mesh of elements (). Tissue layers were represented in the mesh using the thermal properties from Table 1. Absorption data from MC simulations were convolved and converted into the input of the heat transfer model to simulate heat created by laser irradiation. The initial tissue temperature was 37°C (310 K) with contact probe cooling temperature set to 0°C (273 K). A standard Arrhenius integral model was employed to predict thermal injury using published values.28 A single damage parameter, , quantified thermal damage to tissue [Eq. (6)] where () is the experimentally derived frequency factor, is the total heating time, () is the experimentally derived activation energy of transformation (Table 1), () is the universal gas constant, and is the absolute tissue temperature (kelvin). Thermal damage corresponds to . Damage rate increases exponentially when temperature exceeds .Simulations computed thermal damage based on optical, thermal, and damage parameters for the tissues (Table 1). Due to limited availability of damage parameter data, vaginal wall was modeled as smooth muscle, endopelvic fascia as collagen, and urethral wall as aorta tissue. 3.Results3.1.Comparison of Different Optical Clearing Agent MixturesFigure 1 shows optical transmission increases in vaginal tissue at , as a function of time for various OCAs and mixtures. 100% glycerol provided the best result, an optical transmission increase of 61% after 30 min, compared to 100% EG, PG, and DMSO, which yielded increases of 42%, 41%, and 35%, respectively. Vaginal tissue lacks the barrier properties of skin, and hence the additional mixture of DMSO to other OCA solutions tested, which facilitates the perfusion transport process, did not provide improved optical transmission. 3.2.Optical Coherence TomographyComparison of OCT images taken with and without OCA, and at room (22°C) and body temperatures (37°C), shows how diffusion of glycerol in tissue reduces scattering and allows imaging of deeper tissue layers (Fig. 2). For porcine vaginal tissue at 22°C, after 30 min of glycerol application, a 32% increase in optical transmission was measured using the following method. Since gray scale intensity is directly proportional to photon penetration depth, the intensity decrease is equal to a gray scale value of 94. At 22°C, in the initial OCT image (), a intensity decrease was measured at a depth of 0.484 mm. However, after OCA application (), the new , gray scale value of 94 increased to a depth 0.639 mm, which translates to a 32% increase in optical penetration depth with OCA. Using a similar method, at 37°C, an increase in optical transmission of 59% was measured. Improved optical transmission at higher tissue temperatures is achieved from greater permeability of glycerol due to higher molecular kinetic energy, in agreement with previous studies.18 Fig. 2Optical coherence tomography images of porcine vaginal wall in its (a) native state without glycerol, at room temperature, 22°C; (b) after topical application of 100% glycerol for 30 min, at room temperature, 22°C, transmission increased by 32%; (c) native state without glycerol, at body temperature, 37°C; (d) after topical application of 100% glycerol for 30 min, at body temperature, 37°C, transmission increased by 59%; (e) increase in optical transmission using glycerol, for 22°C () and 37°C (); where higher tissue temperature yielded greater perfusion rate of glycerol in tissue and hence increased optical transmission as well. 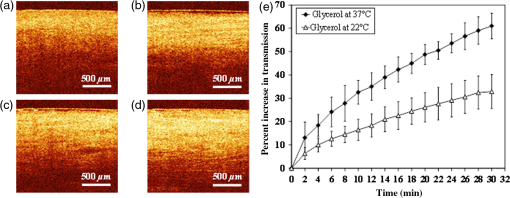 3.3.Reflection SpectroscopyAfter OCA treatment, the tissue reflection spectrum was altered, as observed by a change in color at the tissue surface. For porcine vaginal tissue wall, after 30 min of glycerol, the rapid decrease in reflection in green and blue spectrum and slower decrease in reflection in red spectrum was measured, corresponding to a progressively darker red appearance of the vaginal wall (Fig. 3). This is due to major hemoglobin absorption peaks at 420, 540, and 580 nm, which reduce the amount of reemitted light from tissue compared to the red part of the spectrum. Fig. 3Porcine vaginal wall in its (a) native state and (b) after topical application of 100% glycerol for 30 min, (c) percent decrease in reflection across the visible and near-IR spectrum. Note that the lowest decrease in reflection occurs in the red (600–700 nm), accounting for the change in appearance of the tissue. 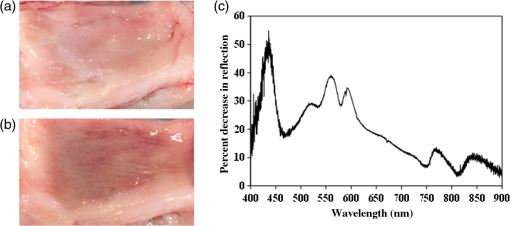 3.4.Computer SimulationsMC simulations predicted that 50% of energy is absorbed by vaginal wall, 49% is absorbed in endopelvic fascia target layer, and only 1% is deposited in urethral wall. This corresponded to a 12% decrease in energy absorbed by the vaginal wall and 12% increase in energy absorbed in the endopelvic fascia layer using OCA, versus without OCA application. After applying glycerol for 30 min, scattering in vaginal wall decreased, enabling photons to penetrate deeper into endopelvic fascia where scattering coefficient is greater (Table 1). Energy deposition as a function of depth is shown in Fig. 4. The initial subsurface peak is due to additional contributions of photons through subsurface scattering. The large peak between the vaginal wall and the endopelvic fascia is due to an increase in the scattering coefficient across the interface. The rapid decline in energy absorbed in the endopelvic fascia is due to the high scattering coefficient. Fig. 4One-dimensional absorbed energy distribution by porcine vaginal tissue at the center of laser irradiation at 5 W, both with OCA (blue) and without OCA (red). 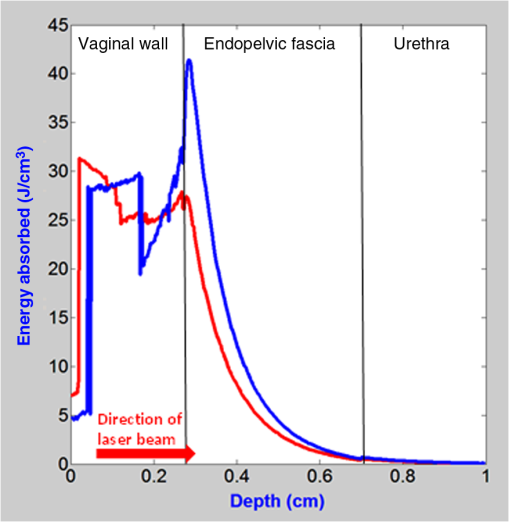 Heat transfer simulations were also conducted. For similar laser power simulated (5 W, 15 s), use of OCA resulted in higher energy deposition in the endopelvic fascia, which translated into a 7°C higher peak temperature than without OCA [Figs. 5(a) and 5(c)]. However, 15 s after laser was turned off, peak tissue temperatures decayed to a similar value of , with tissue including OCA only 0.5°C higher than tissue without OCA [Figs. 5(b) and 5(d)]. Fig. 5(a) Two-dimensional temperature distribution (depth x width) after laser irradiation for 15 s. Internal tissue temperature reached 71°C (344°K) at boundary between vaginal wall and endopelvic fascia, (b) temperature distribution in tissue 15 s after laser irradiation, for transvaginal approach. Peak temperature decreased to 42.8°C (316.0°K) at end of 15 s postoperative cooling time period, (c) temperature after laser irradiation for 15 s with OCA reached 78.1°C (351.3°K), (d) peak temperature decreased to 43.3°C (316.5°K) at end of 15 s postoperative cooling time period. 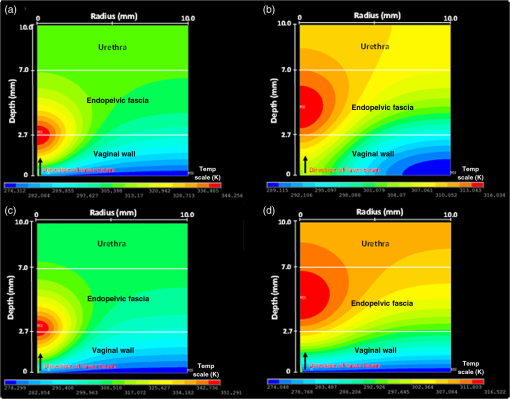 For comparison, the same laser power and time were initially used to contrast thermal damage with and without OCA. Arrhenius integral calculations [Eq. (6)] indicated higher damage in vaginal tissue with OCA () compared to without OCA () (Fig. 6), due to the higher peak temperature in the endopelvic fascia layer with OCA (). Previous clinical SUI studies using radiofrequency (RF) energy targeted 65°C in endopelvic fascia for 30 s, based on temperature versus time data for collagen thermal denaturation and shrinkage.38 This corresponds to a damage parameter of . Hence, the tissue model without OCA required a power increase from 5.0 to 5.35 W, while the OCA model required a power decrease from 5.0 to 4.45 W, to achieve . In practice, OCA treatment is preferred, because it not only enables laser treatment at a lower and hence safer power, but also improves optical penetration depth by 0.5 mm, thus preserving the entire ( thick) vaginal wall during the procedure (Fig. 7). 4.DiscussionRF energy has previously been used for transurethral thermal shrinkage and remodeling of submucosal collagen without tissue necrosis, in bladder neck and proximal urethra as a safe, nonsurgical SUI treatment with improvement in patient quality of life.39,40 However, RF heating is limited and decays rapidly with depth as ( term for resistive heating and term for electric field strength), resulting in a superficial penetration depth due to direct heating of only 1 to 2 mm.41,42 RF probes for SUI therapy therefore require needles inserted through the urethral wall and into submucosal tissue for localized heating, denaturation, and shrinkage of collagen, with saline irrigation of mucosa to prevent overheating. RF therapy is thus more invasive than desired by patients seeking a minimally invasive, nonsurgical treatment. Lasers have recently been used for subablative resurfacing of atrophic vaginal tissue in postmenopausal women, and for treatment of SUI. Both the laser at 43–45 and erbium:YAG laser at 46–50 have been used. Short-term studies appear more promising for vaginal rejuvenation, but also show moderate improvements for SUI. However, these laser wavelengths, adapted from the skin resurfacing field, are limited to an optical penetration depth of tens of micrometers and a thermal treatment zone of less than . Preliminary studies in our laboratory have demonstrated that subsurface thermal denaturation of tissues can be achieved using a deeply penetrating laser wavelength ( or 1075 nm) in conjunction with applied surface cooling, preserving 1 to 2 mm of the tissue surface from thermal necrosis.4,5 Thus, laser denaturation and shrinkage of the endopelvic fascia may potentially produce improved tissue remodeling results similar to the RF approach, but in a less invasive manner with preservation of the vaginal mucosa. Computer simulations utilizing optical, thermal, and damage parameters for vaginal wall, endopelvic fascia, and urethral wall were conducted for a transvaginal endoscopic approach to minimally invasive laser treatment of female SUI, with and without an OCA. By combining contact cooling with OCA, it is possible to preserve the entire 2.7-mm thick vaginal wall from thermal insult. In addition, OCA application translated into use of lower laser power, which may provide a safer and less expensive procedure. Glycerol used in these studies is not only biocompatible, but also OCA effects can be easily reversed with tissue returning to its original state after rehydration. The 100% glycerol solution used in this study is an oversaturated solution, which produces tissue transparency primarily by dehydration. The improved transparency is mainly due to a decrease in tissue thickness and better ordering of the tissue components, rather than refractive-index matching between tissue solid components and interstitial fluids.24 These simulations were based on several assumptions. First, it was assumed that experimental OCA results applied to porcine vaginal tissue will be similar to human vaginal tissue. Second, optical clearing was assumed to produce a decrease only in scattering coefficient, but not absorption coefficient or anisotropy factor. Other studies have reported that the decrease in reduced scattering coefficient is primarily due to an increase in the anisotropy factor () due to structural changes in average collagen fiber size and packing of collagen fibers, rather than an increase in the scattering coefficient.51 We therefore simulated this alternative case as well. However, the results were very similar. MC simulations predicted that 51% of energy is absorbed by vaginal wall, 48% is absorbed in endopelvic fascia target layer, and only 1% is deposited in urethral wall. During thermal simulations, the peak temperature in the endopelvic fascia reached 79.5°C. An incident laser power of 4.43 W was necessary to achieve a damage parameter of . Third, thermal property and damage parameters used in Table 1 were compiled from different sources, introducing a small error in our simulation results. For example, 5 W with OCA produced a peak temperature of 78.1°C in the endopelvic fascia layer during simulations, slightly below the critical damage threshold of 80.4°C provided in Table 1. However, the damage parameter was , a value greater than , which indicates irreversible thermal damage to the tissue. Finally, dynamic optical property values due to changes in temperature and pressure and changes in thermal properties due to tissue perfusion were not included in this model. Despite these limitations, the simulations demonstrate that use of an OCA may further improve treatment depth for thermal remodeling by . This should allow preservation of the entire (2.7-mm thick) vaginal wall during subsurface laser targeting and thermal remodeling of the endopelvic fascia for minimally invasive treatment of female SUI. Future studies will involve histological examination (e.g., hematoxylin and eosin stains) of thermally denatured and remodeled tissue, as well as pivotal in vivo animal studies with functional tests (e.g., Valsalva leak point pressure measurements) to test feasibility of minimally invasive laser therapy for SUI, similar to what has been reported for RF studies.38,48,52 The simulations and results from this study can be utilized as a guide for such studies. 5.ConclusionsThis study used experimental studies and computer simulations to explore whether application of an OCA to vaginal wall can further improve optical penetration depth and completely preserve vaginal wall during subsurface laser treatment of endopelvic fascia. Optical transmission studies showed that glycerol produced a 61% increase in transmission through vaginal wall at body temperature (37°C) versus 32% at room temperature (22°C) over 30 min. MC models of light transport in the tissue layers showed improved energy deposition in endopelvic fascia using glycerol. Without OCA, 62%, 37%, and 1% of energy was deposited in the vaginal wall, endopelvic fascia, and urethral wall, respectively, compared with 50%, 49%, and 1% when using an OCA. Application of an OCA also resulted in a 0.5-mm increase in depth for thermal tissue remodeling, allowing 3 mm of tissue surface to be preserved. AcknowledgmentsThis research was supported by the National Institutes of Health, Grant No. 1R15DK099774. ReferencesD. J. Lightner and N. M. Itano,
“Treatment options for women with stress urinary incontinence,”
Mayo Clin. Proc., 74 1149
–1156
(1999). http://dx.doi.org/10.4065/74.11.1149 MACPAJ 0025-6196 Google Scholar
F. Pesce,
“Current management of stress urinary incontinence,”
BJU Int., 94 8
–13
(2004). http://dx.doi.org/10.1111/bju.2004.94.issue-s1 BJINFO 1464-410X Google Scholar
A. E. Bent and M. T. McLennan,
“Surgical management of urinary incontinence,”
Obstet. Gynecol. Clin. North Am., 25 883
–906
(1998). http://dx.doi.org/10.1016/S0889-8545(05)70048-6 OGCAE8 0889-8545 Google Scholar
R. Ramli et al.,
“Subsurface tissue lesions created using an Nd:YAG laser with a sapphire contact cooling probe,”
Lasers Surg. Med., 35 392
–396
(2004). http://dx.doi.org/10.1002/(ISSN)1096-9101 LSMEDI 0196-8092 Google Scholar
C. H. Chang, C. R. Wilson and N. M. Fried,
“Comparison of four lasers (, 808, 980, and 1075 nm) for noninvasive creation of deep subsurface lesions in tissue,”
Proc. SPIE, 9542 95420G
(2015). http://dx.doi.org/10.1117/12.2183478 PSISDG 0277-786X Google Scholar
C. Demetri, G. Panayi and A. Digesu,
“Ultrasound measurement of vaginal wall thickness: a novel and reliable technique,”
Int. Urogynecol. J., 21 1265
–1270
(2010). http://dx.doi.org/10.1007/s00192-010-1183-4 IUJOEF Google Scholar
A. P. Wieczorek et al.,
“3-D high-frequency endovaginal ultrasound of female urethral complex and assessment of inter-observer reliability,”
Eur. J. Radiol., 81 e7
–e12
(2012). http://dx.doi.org/10.1016/j.ejrad.2010.09.044 EJRADR 0720-048X Google Scholar
L. A. Hardy et al.,
“Computer simulations of thermal tissue remodeling during transvaginal and transurethral laser treatment of female stress urinary incontinence,”
Lasers Surg. Med., Google Scholar
D. Zhu et al.,
“Recent progress in tissue optical clearing,”
Laser Photonics Rev., 7 732
–757
(2013). http://dx.doi.org/10.1002/lpor.2013.7.issue-5 Google Scholar
D. Tuchina et al.,
“Ex vivo optical measurements of glucose diffusion kinetics in native and diabetic mouse skin,”
J. Biophotonics, 8 332
–346
(2015). http://dx.doi.org/10.1002/jbio.v8.4 Google Scholar
M. H. Khan et al.,
“Optical clearing of in vivo human skin: implications for light-based diagnostic imaging and therapeutics,”
Lasers Surg. Med., 34 83
–85
(2004). http://dx.doi.org/10.1002/(ISSN)1096-9101 LSMEDI 0196-8092 Google Scholar
Z. Zhu et al.,
“Investigation of the permeability and optical clearing ability of different analytes in human normal and cancerous breast tissues by spectral domain OCT,”
J. Biophotonics, 5 536
–543
(2012). http://dx.doi.org/10.1002/jbio.201100106 Google Scholar
Q. Zhao et al.,
“Evaluation of ultrasound and glucose synergy effect on the optical clearing and light penetration for human colon tissue using SD-OCT,”
J. Biophotonics, 7 938
–947
(2014). http://dx.doi.org/10.1002/jbio.v7.11/12 Google Scholar
Q. Zhao et al.,
“Concentration dependence of optical clearing on the enhancement of laser scanning optical-resolution photoacoustic microscopy imaging,”
J. Biomed. Opt., 19 036019
(2014). http://dx.doi.org/10.1117/1.JBO.19.3.036019 JBOPFO 1083-3668 Google Scholar
E. A. Genina et al.,
“Optical coherence tomography monitoring of enhanced skin optical clearing in rat in vivo,”
J. Biomed. Opt., 19 021109
(2014). http://dx.doi.org/10.1117/1.JBO.19.2.021109 JBOPFO 1083-3668 Google Scholar
L. M. Oliveira et al.,
“Diffusion characteristics of ethylene glycol in skeletal muscle,”
J. Biomed. Opt., 20 051019
(2015). http://dx.doi.org/10.1117/1.JBO.20.5.051019 JBOPFO 1083-3668 Google Scholar
C. G. Rylander et al.,
“Dehydration mechanism of optical clearing in tissue,”
J. Biomed. Opt., 11 041117
(2006). http://dx.doi.org/10.1117/1.2343208 JBOPFO 1083-3668 Google Scholar
Z. Deng et al.,
“Improvement of skin optical clearing efficacy by topical treatment of glycerol at different temperatures,”
J. Phys., 277 012007
(2011). http://dx.doi.org/10.1088/1742-6596/277/1/012007 Google Scholar
B. Choi et al.,
“Determination of chemical agent optical clearing potential using in vitro human skin,”
Lasers Surg. Med., 36 72
–75
(2005). http://dx.doi.org/10.1002/(ISSN)1096-9101 LSMEDI 0196-8092 Google Scholar
J. M. Hirshburg et al.,
“Molecular basis for optical clearing of collagenous tissues,”
J. Biomed. Opt., 15 055002
(2010). http://dx.doi.org/10.1117/1.3484748 JBOPFO 1083-3668 Google Scholar
A. Bykov et al.,
“Imaging of subchondral bone by optical coherence tomography upon optical clearing of articular cartilage,”
J. Biophotonics, 9 270
–275
(2016). http://dx.doi.org/10.1002/jbio.v9.3 Google Scholar
E. A. Genina, A. N. Bashkatov and V. V. Tuchin,
“Optical clearing of cranial bone,”
Adv. Opt. Tech., 2008 267867
(2008). http://dx.doi.org/10.1155/2008/267867 1687-6393 Google Scholar
T. Son and B. Jung,
“Cross-evaluation of optimal glycerol concentration to enhance optical tissue clearing efficacy,”
Skin Res. Technol., 21 327
–332
(2015). http://dx.doi.org/10.1111/srt.2015.21.issue-3 Google Scholar
L. M. Oliveira et al.,
“Optical clearing mechanisms characterization in muscle,”
J. Innovative Opt. Health Sci., 9 1650035
(2016). http://dx.doi.org/10.1142/S1793545816500358 Google Scholar
H. Ao et al.,
“Thermal coagulation-induced changes of the optical properties of normal and adenomatous human colon tissue in vitro in the spectral range 400–1100 nm,”
Phys. Med. Biol., 53 2197
–2206
(2008). http://dx.doi.org/10.1088/0031-9155/53/8/013 PHMBA7 0031-9155 Google Scholar
G. Muller and A. Roggan, Laser Induced Interstitial Thermotherapy, SPIE Optical Engineering Press, Bellingham, Washington
(1995). Google Scholar
C. L. Tsai, J. C. Chen and W. J. Wang,
“Near-infrared absorption property of biological soft tissue constituents,”
J. Med. Biol. Eng., 21
(1), 7
–14
(2001). IYSEAK 0021-3292 Google Scholar
S. Thomsen, J. A. Pearce,
“Thermal damage and rate processes in biological tissues,”
Optical-Thermal Response of Laser-Irradiated Tissue, 487
–549 2nd ed.Springer, Heidelberg
(2011). Google Scholar
R. L. McIntosh and V. Anderson,
“Comprehensive tissue properties database provided for the thermal assessment of a human at rest,”
Biophys. Rev. Lett., 5
(3), 129
–151
(2010). http://dx.doi.org/10.1142/S1793048010001184 1793-0480 Google Scholar
X. Xu and R. K. Wang,
“Synergistic effect of hyperosmotic agents of dimethyl sulfoxide and glycerol on optical clearing of gastric tissue studied with near-infrared spectroscopy,”
Phys. Med. Biol., 49 457
–468
(2004). http://dx.doi.org/10.1088/0031-9155/49/3/008 PHMBA7 0031-9155 Google Scholar
J. Jiang and R. K. Wang,
“Comparing the synergistic effects of oleic acid and dimethyl sulfoxide as vehicles for optical clearing of skin tissue in vitro,”
Phys. Med. Biol., 49 5283
–5294
(2004). http://dx.doi.org/10.1088/0031-9155/49/23/006 PHMBA7 0031-9155 Google Scholar
A. K. Bui et al.,
“Revisiting optical clearing with dimethyl sulfoxide (DMSO),”
Lasers Surg. Med., 41 142
–148
(2009). http://dx.doi.org/10.1002/lsm.v41:2 LSMEDI 0196-8092 Google Scholar
C. M. Cilip et al.,
“Application of an optical clearing agent during noninvasive laser coagulation of the canine vas deferens,”
J. Biomed. Opt., 15
(4), 048001
(2010). http://dx.doi.org/10.1117/1.3463009 JBOPFO 1083-3668 Google Scholar
V. V. Tuchin,
“Tissue and blood optical immersion by exogenous chemical agents,”
Optical Clearing of Tissue and Blood, 9
–18 SPIE Press, Bellingham, Washington
(2006). Google Scholar
S. L. Jacques,
“Monte Carlo modeling of light transport in tissues (steady state and time of flight),”
Optical-Thermal Response of Laser-Irradiated Tissue, 109
–144 2nd ed.Springer, Heidelberg
(2011). Google Scholar
L. H. Wang, S. L. Jacques and L. Q. Zheng,
“MCML– Monte Carlo modeling of photon transport in multi-layered tissues,”
Comput. Methods Programs Biomed., 47 131
–146
(1995). http://dx.doi.org/10.1016/0169-2607(95)01640-F CMPBEK 0169-2607 Google Scholar
L. H. Wang, S. L. Jacques and L. Q. Zheng,
“CONV– Convolution for responses to a finite diameter photon beam incident on multi-layered tissues,”
Comput. Methods Programs Biomed., 54 141
–150
(1997). http://dx.doi.org/10.1016/S0169-2607(97)00021-7 CMPBEK 0169-2607 Google Scholar
M. S. Wall et al.,
“Thermal modification of collagen,”
J. Shoulder Elbow Surg., 8 339
–344
(1999). http://dx.doi.org/10.1016/S1058-2746(99)90157-X Google Scholar
G. W. Davila,
“Nonsurgical outpatient therapies for the management of female stress urinary incontinence: long-term effectiveness and durability,”
Adv. Urol., 2011 176498
(2011). http://dx.doi.org/10.1155/2011/176498 Google Scholar
J. C. Lukban,
“Transurethral radiofrequency collagen denaturation for treatment of female stress urinary incontinence: a review of the literature and clinical recommendations,”
Obstet. Gynecol. Int., 2012 384234
(2012). http://dx.doi.org/10.1155/2012/384234 Google Scholar
D. L. Lustgarten and P. S. Spector,
“Ablation using irrigated radiofrequency: a hands-on guide,”
Heart Rhythm, 5 899
–902
(2008). http://dx.doi.org/10.1016/j.hrthm.2008.01.003 Google Scholar
C. L. Brace,
“Radiofrequency and microwave ablation of the liver, lung, kidney, and bone: what are the differences?,”
Curr. Probl. Diagn. Radiol., 38 135
–143
(2009). http://dx.doi.org/10.1067/j.cpradiol.2007.10.001 CPDRDS 0363-0188 Google Scholar
S. Salvatori et al.,
“A 12-week treatment with fractional laser for vulvovaginal atrophy: a pilot study,”
Climacteric, 17 363
–369
(2014). http://dx.doi.org/10.3109/13697137.2014.899347 Google Scholar
S. Salvatore et al.,
“Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study,”
Menopause, 22 845
–849
(2015). http://dx.doi.org/10.1097/GME.0000000000000401 Google Scholar
N. Zerbinati et al.,
“Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment,”
Lasers Med. Sci., 30 429
–436
(2015). http://dx.doi.org/10.1007/s10103-014-1677-2 Google Scholar
Z. Vizintin et al.,
“Erbium laser in gynecology,”
Climacteric, 18
(Suppl 1), 4
–8
(2015). http://dx.doi.org/10.3109/13697137.2015.1078668 Google Scholar
U. B. Ogrinc, S. Sencar and H. Lenasi,
“Novel minimally invasive laser treatment of urinary incontinence in women,”
Lasers Surg. Med., 47 689
–697
(2015). http://dx.doi.org/10.1002/lsm.v47.9 LSMEDI 0196-8092 Google Scholar
N. Fistonic et al.,
“Minimally invasive, non-ablative Er:YAG laser treatment of stress urinary incontinence in women– a pilot study,”
Lasers Med. Sci., 31 635
–643
(2016). http://dx.doi.org/10.1007/s10103-016-1884-0 Google Scholar
Y. W. Tien et al.,
“Effects of laser procedure for female urodynamic stress incontinence on pad weight, urodynamics, and sexual function,”
Int. Urogynecol. J., 1
–8
(2016). http://dx.doi.org/10.1007/s00192-016-3129-y Google Scholar
J. I. Pardo, V. R. Sola and A. A. Morales,
“Treatment of female stress urinary incontinence with Erbium-YAG laser in non-ablative mode,”
Eur. J. Obstet. Gynecol. Reprod. Biol., 204 1
–4
(2016). http://dx.doi.org/10.1016/j.ejogrb.2016.06.031 EOGRAL 0301-2115 Google Scholar
R. Samatham, K. G. Phillips and S. L. Jacques,
“Assessment of optical clearing agents using reflectance-mode confocal scanning laser microscopy,”
J. Innovative Opt. Health Sci., 3 183
–188
(2010). http://dx.doi.org/10.1142/S1793545810001064 Google Scholar
P. S. Edelstein,
“A preclinical study of nonsurgical radiofrequency collagen remodelling for treatment of stress urinary incontinence,”
Expert Rev. Med. Dev., 3 743
–748
(2006). http://dx.doi.org/10.1586/17434440.3.6.743 1743-4440 Google Scholar
BiographyChun-Hung Chang is currently a PhD student in the Optical Science and Engineering Program at the University of North Carolina at Charlotte. Erinn M. Myers is currently a physician specializing in female pelvic medicine and reconstructive surgery with the Women’s Center for Pelvic Health at Carolinas Medical Center. Michael J. Kennelly is currently the director of the Women’s Center for Pelvic Health at Carolinas Medical Center. Nathaniel M. Fried is currently a professor in the Department of Physics and Optical Science at the University of North Carolina at Charlotte and an adjunct faculty member in the McKay Department of Urology at Carolinas Medical Center. His research interests include therapeutic and diagnostic applications of lasers in urology. |