|
|
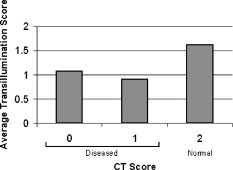
1.IntroductionSinusitis affects approximately 31 million individuals in the United States and accounts for greater than $5.8 billion in direct and indirect health care costs annually.1 Data suggests that sinusitis is the most commonly reported chronic disease.2 Although many specialists may play a role in the management of sinusitis, primary care physicians are called on to diagnose and treat up to 87% of the cases.3 Despite its prevalence, sinusitis remains a difficult diagnosis for primary care physicians to make. In an effort to help simplify the clinical diagnosis, in 1997, the American Academy of Otolaryngology—Head and Neck Surgery Task Force on Rhinosinusitis established a list of major and minor criteria that characterize the disease.4 Nonetheless, there has never been a solid body of evidence to support the Task Force on Rhinosinusitis’s symptom-based definition of sinusitis, and in fact, studies have found that the symptom-based definition may overestimate disease.5 Chronic sinusitis is especially difficult to diagnose, as its symptoms are vague and/or may be shared by other diseases such as allergic rhinitis, vasomotor rhinitis, migraine, myofacial pain syndromes, temporomandibular joint disorders, etc. Moreover, clinical diagnosis depends on the patient’s ability to convey a cogent history (which may be difficult when the patient is a child or is not fluent in English) and the clinical acumen of the physician (which may be hindered by the limited consultation time available in today’s managed care environment). Nonetheless, failure to diagnose sinusitis can lead to further patient morbidity, potentially serious complications, and unnecessary health care expenditures when the diagnosis is delayed or missed. The challenge of diagnosing sinusitis in the primary care setting has led to an overuse of plain film x rays and computed tomography (CT). Obviously, CT improves the accuracy of diagnosis, but it is not cost effective as a screening examination,6 even when employed using a screening protocol. As such, there is a need for a simple office-based diagnostic technique to aid in the diagnosis of sinusitis without the cost and radiation risk of conventional radiologic imaging. Historically, the office-based objective study used to aid in the diagnosis of sinusitis was transillumination. This technique involved the direct placement of an incandescent light source on a maxillary or frontal sinus wall to detect fluid in the normally air-filled sinus. Fluid accumulation results in increased absorption of light and decreased light transmission. Traditional transillumination proved to be largely inaccurate, however, and was discarded at the earlier part of the twentieth century with the advent of radiography.7, 8, 9 Recent advancements in the field of optics have provided an exciting and cost-effective means by which to address numerous challenges in the field of medicine. In this study, we constructed a near-infrared (NIR) imaging system for the sinuses. NIR light is poorly absorbed by water and hemoglobin, the main constituents of biological tissues,10, 11 permitting enhanced illumination of deep-tissue structures because of the deeper optical penetration depth. Because the eye cannot detect NIR light, infrared imaging devices are needed to detect the signal. We used a low-cost charge-coupled device (CCD) camera sensitive to NIR wavelengths to capture and record images. The objective of this pilot study was to determine whether NIR imaging may have potential as a technology to aid in the diagnosis of maxillary sinusitis by comparing NIR images with CT imaging. The long-term objective of our research is to develop low-cost NIR imaging technology to aid in the diagnosis of sinus disease particularly in primary care settings. 2.Materials and MethodsOur NIR imaging system consists of two basic components: an NIR light source and an imaging detector. The fundamental elements of our system have been described previously,12 and only a brief overview is provided here. The light source (Fig. 1 ) is designed to provide transpalatal illumination of the maxillary sinuses. Structurally, the light source is shaped like a spoon with a handle at one end and is constructed from clear acrylic and polystyrene. Two arrays of four light emitting diodes (LEDs; Roithner Lasertechnik, Vienna, Austria) are enclosed by a polystyrene shell. One array emits light at a wavelength of , and the other emits at . These specific LEDs were selected based on a combination of cost and pilot experiments that evaluated their tissue penetration depth. Fig. 1NIR transillumination light source device consisting of two rows of NIR light emitting diodes surrounded by an acrylic casing. 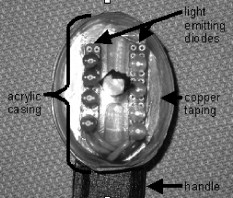 The images were acquired using a silicon-based CCD video camera whose infrared filter was removed to detect the NIR signal (Marlin P. Jones and Associates, Lake Park, Florida). The output from the camera interfaces with a USB port via an RCA-to-USB adapter, allowing NIR images to be captured onto a notebook PC using video capturing software (Pinnacle Systems, Inc., Mountain View, California). The total cost of the system, including the light source and detector but excluding the PC, is less than $100. Subjects were enrolled in our study in accordance with the UC Irvine Institutional Review Board. Informed written consent was obtained from all participating subjects, who were recruited among patients undergoing management of sinusitis or other paranasal sinus diseases at the Otolaryngology—Head and Neck Surgery Clinic at the University of California at Irvine Medical Center. The inclusion criteria were (1) patient age 15 or older, and (2) patients had undergone or were anticipated to undergo CT imaging; otherwise, subjects were not discriminated on the basis of clinical findings. NIR imaging was performed in an examination room at the UC Irvine Medical Center. Subjects were seated approximately in front of the CCD camera, which was secured to a tripod that allowed adjustment of height. For hygiene purposes, the NIR light source was covered with a sterile, disposable plastic bag that was discarded after each use. Patients placed the light source against their hard palates and were asked to cover their mouths with their hands to reduce direct backscattering of light out of the oral cavity and directly into the camera. The room was then completely darkened, thus minimizing the amount of ambient visible light that might saturate the detector. Video of each patient’s NIR imaging pattern was recorded onto a notebook PC for later analysis. During recording, subjects were instructed to rotate, flex, and extend their heads in order to capture images from various perspectives. The total imaging duration for each patient was approximately . When possible, serial images were obtained from patients as they underwent medical or surgical treatment (e.g., endoscopic sinus surgery). Comparisons were made between patients’ NIR imaging and data obtained from CT scans. For quantitative comparisons, each patient’s maxillary sinus was given two scores, one determined by data obtained from CT imaging and the other by data obtained from similar analysis of the NIR images. CT scoring was based on a modification of the Lund MacKay scoring system often used for sinusitis research.13 On CT, maxillary sinuses were scored from 0 to 2 based on the degree of aeration present in the indicated sinus: each maxillary sinus was given a 2 if it was completely aerated (indicative of a normal sinus), a 1 if there was peripheral mucosal thickening, or a 0 if there was 100% opacification. Maxillary sinuses were similarly scored based on the pattern and degree of NIR signal penetration (Fig. 2 ): each maxillary sinus was given a 2 if light penetrated through the entire maxilla to the border of the infraorbital rim, a 1 if there was reduced signal intensity over the maxilla, or a 0 if there was no perception of light over the maxilla. In order to further stratify NIR imaging scores, a point was deducted from the score of those maxillary sinuses that displayed significantly weaker signal compared to the contralateral sinus despite equal scores using the preceding system. Each patient’s NIR imaging pattern was scored independently by three blinded otolaryngologists on the faculty at UC Irvine. Fig. 2Schematic demonstrating NIR transillumination pattern scoring. Each patient’s maxillary sinus was scored on a 0-to-2 scale based on the degree of NIR light penetration into the sinus. 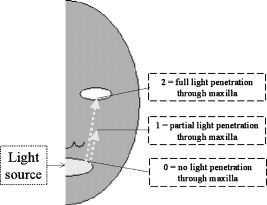 The NIR image score was averaged for each patient’s maxillary sinus and then divided into three groups based on CT score. ANOVA statistical analysis was performed on this data. Additionally, opacified maxillary sinuses (CT or 1) were grouped and compared to normal maxillary sinuses (CT ) using two-tailed -test statistical analysis. Standard significance criteria were used (i.e., -value less than 0.05). 3.ResultsBetween May 2003 and June 2005, a total of 35 patients were enrolled in our study and underwent NIR imaging. Fourteen patients did not undergo CT imaging as originally planned (e.g., were lost to follow-up or missed their appointment for CT scan). The remaining 21 patients did undergo CT imaging. The average age of these 21 patients was old ( old); 55% were male and 45% were female. Sixty-two percent were white, 24% were Asian, and 14% were Hispanic. These 21 patients yielded a total of 42 maxillary sinus NIR imaging patterns with corresponding CT data. Of these 42, 5 were completely opacified (CT ), 24 had peripheral mucosal thickening (CT ), and 13 were completely aerated (CT ). Several trends were observed on comparison of NIR images with CT scans. Subjects without CT evidence of maxillary sinus disease typically displayed diffusely strong NIR signal patterns throughout the maxilla (Fig. 3 ). The NIR signal was often robust in the region immediately below the eyes as NIR light penetrated through the orbital floor, was diffusely scattered by periorbital fat, and escaped via the lower lid. Patients with extensive bilateral maxillary sinusitis, on the other hand, typically displayed relatively dim NIR signal patterns (Fig. 4 ). NIR light penetration through their maxillary sinuses was usually either significantly diminished or absent. Of note, the strong NIR signal immediately below the eyes that characterized disease-free patients was absent. In subjects that had extensive unilateral maxillary sinus disease, the NIR signal pattern was asymmetrical, with diminished signal intensity on the affected side as compared to the unaffected side (Fig. 5 ). Last, NIR imaging was used to follow the two patients that underwent endoscopic sinus surgery for treatment of their sinusitis. Postoperative NIR images clearly revealed increased light penetration through the maxilla as compared to preoperative images (Fig. 6 ). Fig. 3(a) NIR transillumination pattern of -old Caucasian female with no history of nasal problems with (b) corresponding CT scan revealing bilaterally aerated maxillary sinuses. Note the diffusely strong transillumination of midface structures with increased signal intensity along the infraorbital rim. 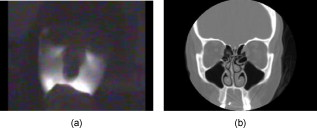 Fig. 4(a) NIR transillumination pattern of -old Asian male with a diagnosis of chronic bilateral maxillary sinusitis with (b) corresponding CT scan revealing significant bilateral mucosal thickening of maxillary sinuses. Note the relatively dim transillumination pattern with absence of NIR light penetration into the maxillary sinuses. 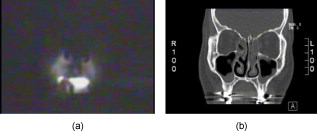 Fig. 5(a) NIR transillumination pattern of -old Caucasian male with a diagnosis of unilateral maxillary sinusitis with (b) corresponding CT scan revealing total opacification of right maxillary sinus. Although subtle, note the relatively dim transillumination pattern of the right midface regions as compared to left, with particularly diminished light penetration through the right infraorbital rim.  Fig. 6(a) Preoperative and (b) postoperative transillumination patterns taken from a -old Caucasian male who underwent surgery for chronic bilateral maxillary sinusitis. Note increased postoperative light penetration through maxillary sinuses with signal abutting infraorbital rim.  There was excellent agreement among the three otolaryngologists in assigning NIR scores. In 33 out of 42 (79%) maxillary sinuses, the otolaryngologists assigned identical NIR scores. In the remainder of cases, the discrepancy between the otolaryngologists’ assigned NIR scores was within one. In no case was a subject’s maxillary sinus assigned an NIR score of both 0 and 2. Our analysis revealed a lower average NIR score for those maxillary sinuses that were totally ( , ) or partially opacified ( , ) as compared to those maxillary sinuses that were totally aerated ( , ) (Fig. 7 ) per CT imaging. ANOVA statistical analysis revealed that these values were significantly different . Moreover, -test statistical analysis revealed a significant difference between the average NIR score of opacified maxillary sinuses with CT scores of 0 or 1 ( , ) and completely aerated maxillary sinuses . 4.DiscussionThe means of diagnosing sinusitis has evolved with technology. In the early part of the twentieth century, transillumination was the sole available imaging modality; however, visualization of the sinuses was poor, and the technique proved to be largely unreliable (both insensitive and nonspecific). With the advent of radiography, plain-film x rays became the standard diagnostic test, and the diagnosis of sinusitis was improved. Today, CT has supplanted x rays; however, its use in the management of sinusitis has been limited mainly to assisting in planning surgical therapy or to evaluating for possible malignancy. Moreover, these studies are costly and involve ionizing radiation, and thus cannot be used serially to gauge the response to therapy. There is no simple, inexpensive, and safe method to accurately confirm the presence of sinus disease. While the clinical diagnosis of sinusitis can be performed relatively easily by otolaryngologists, for other health care practioners (e.g., primary care physicians and nurse practitioners), making this diagnosis remains a substantial challenge, and therefore, patients are often relegated to a pathway of unnecessary imaging studies and antibiotics. A possible solution to this problem is the use of NIR imaging, which is a logical and elegant descendant of the primitive transillumination techniques that arose at the end of the nineteenth century. Our initial results using this technology suggest that air- and fluid-filled maxillary sinuses can be distinguished by their different NIR image patterns, with opacified sinuses yielding significantly lower NIR imaging scores than aerated sinuses. On the other hand, the mean NIR imaging scores were similar in patients with mucosal thickening (0.90) and total opacification (1.07) of their maxillary sinuses. This result could simply be the consequence of a limited number of subjects with total opacification of their maxillary sinuses. Moreover, three of the five totally opacified maxillary sinuses had a normally aerated contralateral sinus. Because light scatters in turbid media, it is possible that the average score of the totally opacified group may be elevated due to the scattering of light across the nasal septum and into the opposite maxilla. Of note, mucosal thickening and total opacification may be potentially separated using varying NIR wavelengths, as scattering and absorption in tissues is wavelength dependent. Regardless, mucosal thickening and opacification are both indicative of abnormal sinus function, and differentiating sinuses with these findings from well-aerated sinuses is more important clinically. This study is not the first to apply NIR light toward the diagnosis of sinus disease. Recently, Mansfield attempted to identify perfusion abnormalities in patients with maxillary sinusitis using NIR hyperspectral imaging.14 Unfortunately, the authors were unable to identify perfusion differences between healthy patients and those with acute maxillary sinusitis. In this study, however, NIR light was both applied and measured externally to the maxillary sinuses rather than used to transilluminate them. Wittek and Beuthan, on the other hand, initially described their technique of IR transillumination several years ago.15 Later, collaborators correlated findings with CT and discussed its potential use in the management of sinus disease.16 These studies, nonetheless, included only a few patients, and the comparisons made between IR transillumination and CT were of a purely qualitative, subjective nature. Moreover, the authors in these studies used multiwavelength sources and detectors, whereas our system is limited to lights of certain wavelengths selected for their optimal tissue penetration. The potential advantages of NIR transillumination are multiple: (1) it is safe for patients and, unlike CT or x ray, does not utilize ionizing radiation; (2) it is only minimally invasive; (3) it allows for real-time acquisition of results, which can be digitally recorded and archived for future reference; (4) it is inexpensive to manufacture and, moreover, can be made easily compatible with existing portable power sources already employed in primary care clinics (such as otoscope hand pieces available in virtually every primary care clinic); and (5) it can be performed in normal ambient light if used with the proper optical filter. An obvious shortcoming of the current NIR imaging system, however, is that it is limited to the interrogation of the maxillary sinuses and, potentially, the frontal sinuses; signals from the sphenoid and ethmoid sinuses, which reside deeper in the skull, may not be spatially resolved using this technique. Nevertheless, the literature suggests that the maxillary sinuses are the most commonly involved in sinus disease. This is because the maxillary sinuses are the largest of the sinus cavities and are likely the most frequently involved in sinus disorders due to their participation in the respiratory system (causing them to be subject to the same infectious and inflammatory processes) and close contact with the superior dental arch.17 There are several potential applications for this technology. For the nonspecialist practitioner, this technology would allow rapid and simple diagnostics of the paranasal maxillary or frontal sinuses without the cost or risk of standard radiography. This technology may be useful for the pediatric population, in which there is a great hesitancy to submit young children to radiographic examination (although the size and development of these patients sinuses may hinder the ability to obtain images that correlate with structural anatomy). Furthermore, once a patient has been diagnosed with sinusitis, this technology could be a simple and safe means to monitor the clinical response to medical or surgical therapy. Significant further work needs to be done in order to demonstrate the true clinical utility of NIR sinus imaging. One future research goal is to optimize the use of NIR wavelengths to yield the most clinically informative images. In this study, we chose specific LED wavelengths based on pilot experiments designed to optimize tissue penetration. However, like other disease processes such as cancer, sinusitis is likely spectrally sensitive, as the propagation of light in tissues depends on the wavelength-dependent optical properties of the tissue. Additional LED wavelengths may enhance discrimination between diseased and normal sinuses by providing an internal reference (i.e., comparison of one wavelength to another) and/or by preferential absorption from fluids/structures. We emphasize that one of our design goals was to maintain very low instrument cost , and thus a basic system that can be expanded is a reasonable starting point. We also plan to model light propagation in the head by using transport-based light propagation models with anatomical detail provided by the CT scans. While our goal is not to perform image reconstructions or use the CTs as image priors, simple modeling studies can help determine the sensitivity of the NIR light to various diseased states. Last, image processing algorithms may help yield valuable clinical information by quantifying image features and allowing longitudinal comparisons that may detect small changes over time. In our pilot study, we merely looked to compare NIR imaging findings with CT data rather than clinical symptoms, as this is the first step in developing the technology. Long-term, significant device refinement and large clinical trials will be needed to determine the sensitivity and specificity of this technique, bearing in mind that there are several clinical entities that may lead to false positive results with NIR imaging (e.g., viral infections, structural abnormalities of the sinuses, and mucosal irregularities). Moreover, children will need to be included in future studies to determine the efficacy of NIR transillumination in this unique population. Last, NIR transillumination may also be used to study the frontal sinuses, although these sinuses are of less significance than the maxillary sinuses in terms of disease rates. AcknowledgmentsThis work has been made possible through support from the National Institutes of Health–sponsored Laser Medical and Microbeam Program, the UC Irvine Health Sciences Partners, the Irvine Head and Neck Research Foundation, the General Clinical Research Center at UC Irvine, and the Stern Foundation. The authors would like to thank Gigi Au, Mai Thy Truong, and Rodney Engel, whose efforts were key in the development of this technology. ReferencesM. S. Benninger, B. J. Ferguson, J. A. Hadley, D. Hamilos, M. Jacobs, D. Kennedy, D. Lanza, B. Marple, J. Osguthorpe, and J. Stankiewicz,
“Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology,”
Otolaryngol.-Head Neck Surg., 129 S1
–32
(2003). https://doi.org/10.1016/S0194-5998(03)01397-4 0194-5998 Google Scholar
V. Benson and M. A. Marano,
“Current estimates from the 1993 National Health Interview Survey,”
10 190
(1994) Google Scholar
“National disease and therapeutic index,”
487
–488
(1988–1989) Google Scholar
D. D. Lanza and D. D. Kennedy,
“Adult rhinosinusitis defined,”
Otolaryngol.-Head Neck Surg., 117 S1
–7
(1997). https://doi.org/10.1016/S0194-5998(97)70001-9 0194-5998 Google Scholar
J. A. Stankiewicz and J. M. Chow,
“A diagnositic dilemma for chronic rhinosinusitis: definition accuracy and validity,”
Am. J. Rhinol., 16 199
–202
(2002). 1050-6586 Google Scholar
J. A. Stankiewicz and J. M. Chow,
“Cost analysis in the diagnosis of chronic rhinosinusitis,”
Am. J. Rhinol., 17 139
–142
(2003). 1050-6586 Google Scholar
J. W. Williams Jr., D. L. Simel, L. Roberts, and G. P. Samsa,
“Clinical evaluation for sinusitis: making the diagnosis by history and physical examination,”
Ann. Intern Med., 117 705
–710
(1992). 0003-4819 Google Scholar
F. W. Otten and J. J. Grote,
“The diagnostic value of transillumination for maxillary sinusitis in children,”
Int. J. Pediatr. Otorhinolaryngol., 18 9
–11
(1989). https://doi.org/10.1016/0165-5876(89)90225-5 0165-5876 Google Scholar
E. R. Wald, D. Chiponis, and J. Ledesma-Medina,
“Comparative effectiveness of amoxicillin and amoxicillin-clavulanate potassium in acute paranasal sinus infections in children: a double-blind, placebo-controlled trial,”
Pediatrics, 77 795
–800
(1986). 0031-4005 Google Scholar
A. Hale and B. Querry,
“Optical constants of water in the wavelength region,”
Appl. Opt., 12 555
–563
(1973). https://doi.org/10.1364/AO.12.000555 0003-6935 Google Scholar
V. Prapavat, J. Beuthan, M. Linnarz, O. Minet, J. U. G. Hopf, and G. J. Mueller,
“IR diaphonoscopy in medicine,”
Proc. SPIE, 2081 154
–167
(1993). https://doi.org/10.1117/12.166821 0277-786X Google Scholar
U. Mahmood, R. Dehdari, A. E. Cerussi, Q. Nguyen, T. Kelley, B. J. Tromberg, B. J. Wong,
“Near-infrared transillumination of the maxillary sinuses: overview of methods and preliminary clinical results,”
Proc. SPIE, 5686 333
–339
(2005). https://doi.org/10.1117/12.604703 0277-786X Google Scholar
V. J. Lund and D. W. Kennedy,
“Quantification for staging analysis,”
Ann. Otol. Rhinol. Laryngol. Suppl., 167 17
–21
(1995). 0096-8056 Google Scholar
C. D. Mansfield, E. M. Attas, and R. M. Gall,
“Evaluation of static thermal and near-infrared hyperspectral imaging for the diagnosis of acute maxillary rhinosinusitis,”
J. Otolaryngol., 34 99
–108
(2005). https://doi.org/10.2310/7070.2005.04056 0381-6605 Google Scholar
G. Wittek and J. Beuthan,
“Infrared diaphanoscopy (IRD)—a choice diagnostic procedure? Preliminary results of the clinical testing (German),”
Kinderaerztl. Prax., 58 581
–585
(1990). 0023-1495 Google Scholar
V. Prapavat, M. Linnarz, J. Hopf, J. Beuthan, M. Becker, G. J. Mueller, H. H. Scherer,
“Endoscopic infrared diaphonoscopy: its use and feasibility in diagnostic and treatment procedure for paranasal sinus disease,”
Proc. SPIE, 2131 83
–87
(1994). https://doi.org/10.1117/12.180761 0277-786X Google Scholar
R. Peynegre and P. Rouvier,
“Anatomy and anatomical variations of the paranasal sinuses: influence on sinus dysfunction,”
Diseases of the Sinuses: A Comprehensive Textbook of Diagnosis and Treatment, 3
–32 Humana Press, Totowa, NJ
(1996). Google Scholar
|